Feature
Article
Dr. Laurence Baskin discusses robotic pediatric urological surgery at UCSF
Author(s):
"Robotic surgery has some major advantages. One that rises to the top is that your magnification is anywhere from 10x-15x higher," according to Laurence S. Baskin, MD.
Laurence S. Baskin, MD

In this article, Laurence S. Baskin, MD, gives an overview of the pediatric urology robotics program at the University of California, San Francisco (UCSF). Baskin is a professor of Urology and chief of pediatric urology and holds the Frank Hinman, Jr., MD Distinguished Professorship in Pediatric Urology at UCSF.
We are now in "version 2.0"of our pediatric urology robotic program at UCSF, which started 8 years ago when we moved to our new free-leaning children's hospital in Mission Bay, which is next to our women's and cancer hospital. What's nice is we now have 4 da Vinci Xi robots; all having been upgraded from the SI version. We have excellent support from our adult urologic colleagues who've helped jump-start our program and continue to support our team for complex robotic cases. If there are any glitches or issues with a robot, there are multiple surgeons and support staff who are immediately available to troubleshoot.
"Version 1.0" of the pediatric urology robotic program occurred more than 20 years ago. We had the first robot on the West Coast at our Parnassus Campus. We were able to do about 50 cases, and then the robot moved with our cancer doctors across town to the UCSF Mt Zion Cancer center, and we lost access except for children over 16. This required us to became more facile laparoscopically. Eight years ago, when we moved to our new children’s hospital at UCSF Mission Bay, we got the robots back and our team consisting of Drs. Hillary Copp, Dr. Yi Li and I were again up and running.
I would say that our bread-and-butter case has been robotic pyeloplasty for ureteropelvic junction obstruction, which I think is pretty much true for North America as well as in other countries. If we really step back, we did have initial trepidation about robotic pyeloplasty, because we changed the operation from a retroperitoneal operation to an intraperitoneal operation. We worried about the long-term issues with intraperitoneal laparoscopic surgery. It turns out there probably aren't any, which is great news. The operation is certainly advantageous especially for older patients in respect to recovery time. As opposed to being out of action for 4 to 6 weeks and not being able to play sports or go back to school, they're pretty much back in school after a couple of days, and they're back to sports within a week. This also means less time off work for caregivers. That's a huge advantage.
In respect to smaller scars, I am not sure that makes a difference. We did a clinical research study where we measured scar size and asked patients and families to complete a validated survey about their scar acceptance. We compared patients who had either robotic or laparoscopic, surgery to those who had open surgery.1 It turned out nobody really cared about their scar. All they really wanted was to be better. In other words, they wanted their kidney unblocked and not to worry about their health. So, I personally think the scar issue is a bit overrated and should not be the major reason to embark on robotic/laparoscopic surgery vs open surgery.
Robotic surgery has some major advantages. One that rises to the top is that your magnification is anywhere from 10x-15x higher. When I compare that with using loupes for open surgery, where standard loupes give you 2.5x or 3x, so right away, you've got this huge magnification advantage. When placing sutures, you remain critical but compared with what would be happening with open surgery using loupes, you're just on a different level of being able to be exact in where your suture placement is and where your anatomical dissection is.
REPORT CARD
Report Card on Robotic Surgery
Pyeloplasty for UPJ: A
Complex rare pediatric pelvic pathology: A
High UG Sinus, Prostatic Utricle,
Rectal Duplication
Ectopic Ureters /Ureteroceles with non-functional upper pole: B
Urachal Abnormalities: B
Ureteral Reimplant: C
I'm going to give our report card for robotic pyeloplasty and where we think it fits in over our experience of about 200 robotic cases since we started UCSF Version 2.0 back at Mission Bay. I would give pyeloplasty an "A" and put that on the top of our list for patients who have a uretero-pelvic junction obstruction. In pediatrics, there are really 3 major indications for pyeloplasty.
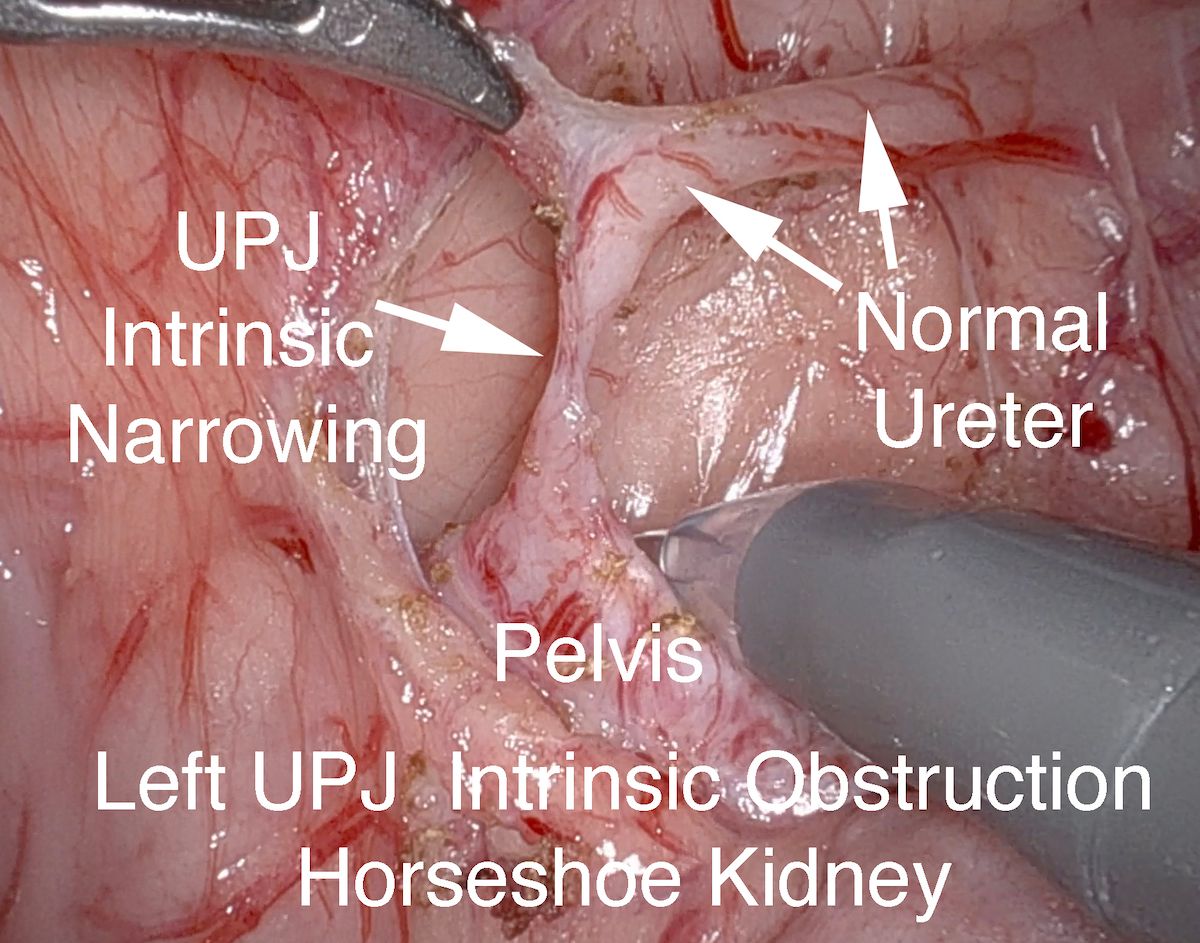
Figure 1

1. Intrinsic narrowing of the ureter causing a UPJ obstruction (Figures 1 and 2). These patients typically present with a prenatal diagnosis found in utero that is confirmed postnatally with follow-up ultrasound (SFU grade IV or UTD 3) and diuretic Lasix renogram. Our bias is that fixing the kidney blockage basically gets closure for the family.
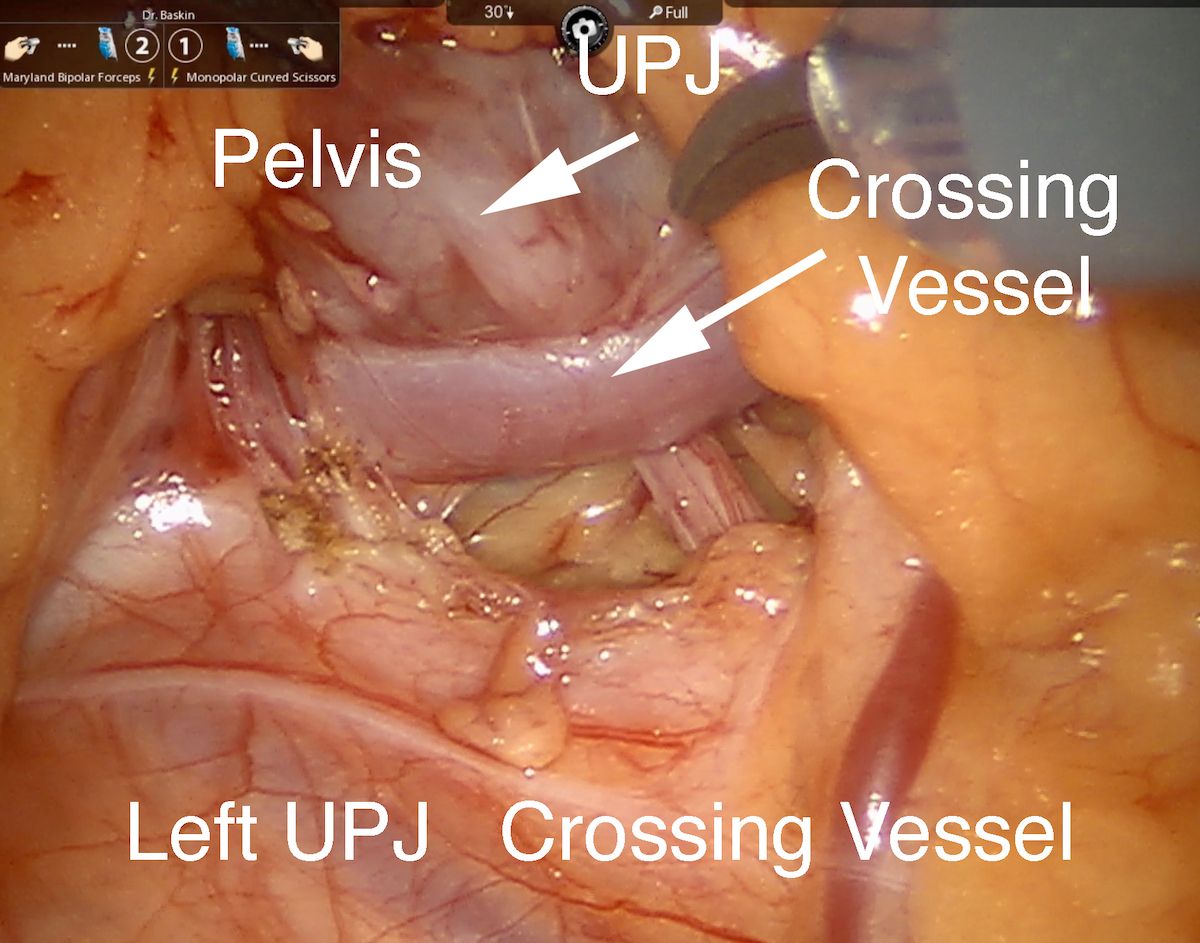
Figure 2
2. We would contrast that to a less common but clearly significant group of patients who are older by nature who present with pain, who have a crossing low pole accessory vessel (Figure 3). This is typically more common in the adult population than in the pediatric and adolescent population. In this group of patients, when you do a robotic transperitoneal approach as opposed to open retroperitoneal, the anatomy is very clear, and it's very hard to miss a crossing vessel.
Figure 3
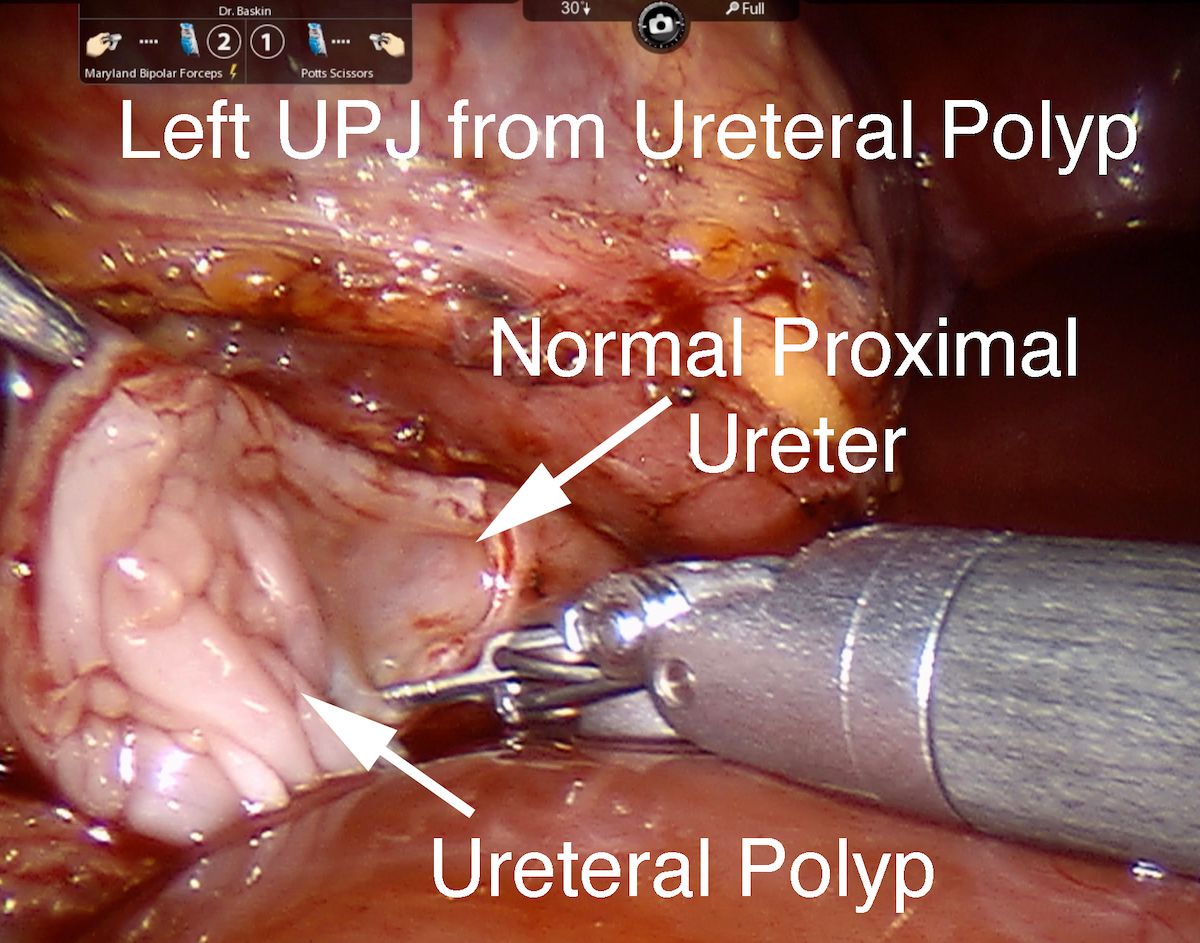
3. The third group of patients that occurs in our practice about once a year or so are the unsuspected patient where they typically have intermittent pain and when you go in, you don't find a crossing vessel, which can be very anxiety provoking because the anatomy looks relatively normal. But when you open the ureter at the ureteropelvic junction, you find a ureteral polyp (Figure 4), which is benign, other than the fact it's causing pain. The polyp tends to be isolated where you can resect the polyp and abnormal ureter. On rare occasions, these patients will require a follow-up ureteroscopic inspection and laser of some recurrent polyps.
Figure 4
For robotic pyeloplasty we leave a double J stent post-operatively for 4 to 6 weeks. We use a 3-port technique with the Xi. We've evolved a bit since we first started performing robotic pyeloplasty. At first, we used an accessory port, which we don't typically use, except in rare circumstances, typically on the right side for exposure. We used to do a cystoscopy or ultrasound at the end of the case to confirm stent placement, but the stent was always in the right position and so we've eliminated that. We do leave a Foley catheter overnight, and the patients typically go home the next morning, so it's a 23-hour stay. We haven't been bold enough to try to send them home the same day because we just don't see a reason that this is going benefit the patient and family. We have eliminated the use of narcotics and have just used Tylenol and ibuprofen. We do routinely perform retrograde pyelograms with specific attention to documenting non-visualization of the ureter on sonogram (or CT scan when obtained).
Figure 5A
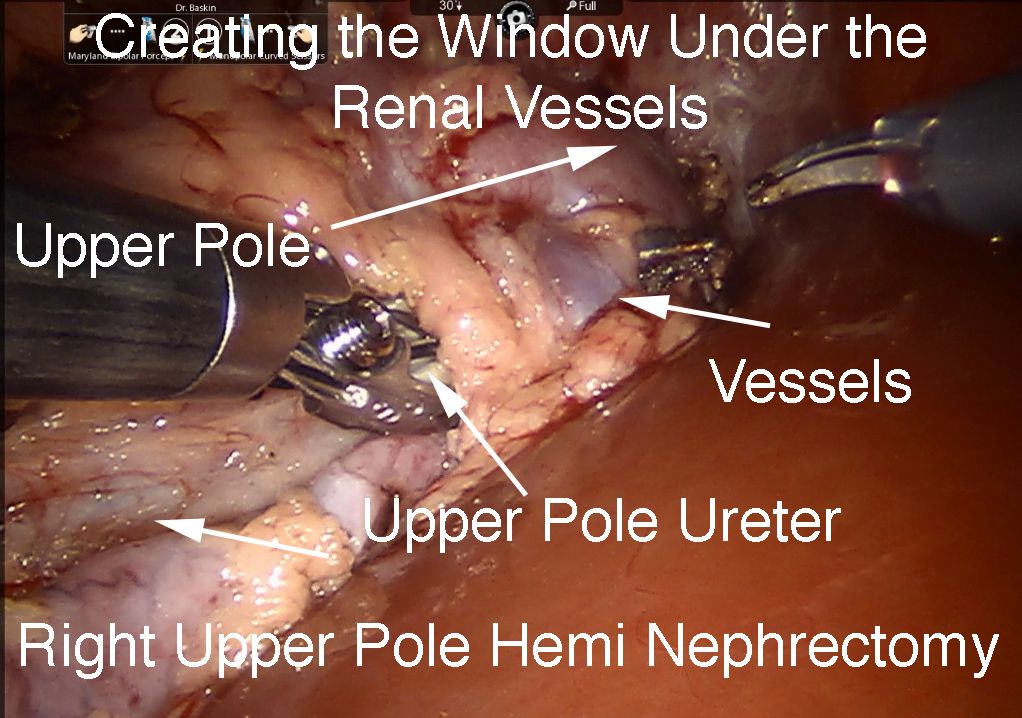
Figure 5B

Another group, which I would also rate as appropriate for robotic surgery, but also appropriate for straight laparoscopic surgery, is in patients who have a duplex system with an ectopic ureter or ureterocele with a nonfunctional upper pole system without lower pole reflux. These patients benefit from the classic treatment of upper pole heminephrectomy (Figure 5 A and B). We have approached this both straight laparoscopic, which I think is fine, but we've also used the robot for this, which also works just as well, using the robotic ligature for the removal of the small nonfunctional kidney. I'd give that an "A-" or "B+," with the "B+" meaning that you could do it laparoscopically and you don't necessarily need the robot, in contrast to pyeloplasty, where the robot facilitates the suturing.
What are other indications for robotic pediatric urologic surgery? We have used this in patients who have megaureters that are obstructed, and I would give that a "C" because it's just not very common. We have not embraced standard ureteral reimplantation for 2 reasons. We think the indication for standard ureteral reimplantation surgery has become much narrower than, for example, 10 years ago, or even 20 to 30 years ago, when it really was one of the founding and most common surgeries of pediatric urology. The published data, with a 60% to 80% success rate, is much different than the greater than 90% success rate that we see with open surgery. Also, most patients with primary reflux respond to endoscopic treatment or watchful waiting.
Most patients that we see now have complex ureteral issues that require more complex reconstruction; for example, an ectopic ureter or a huge ureter with a ureterocele. And for kidney, where there is decent function upper pole function, we have basically gone to the classic Pfannenstiel transverse incision and performed lower tract surgery.
Figure 6
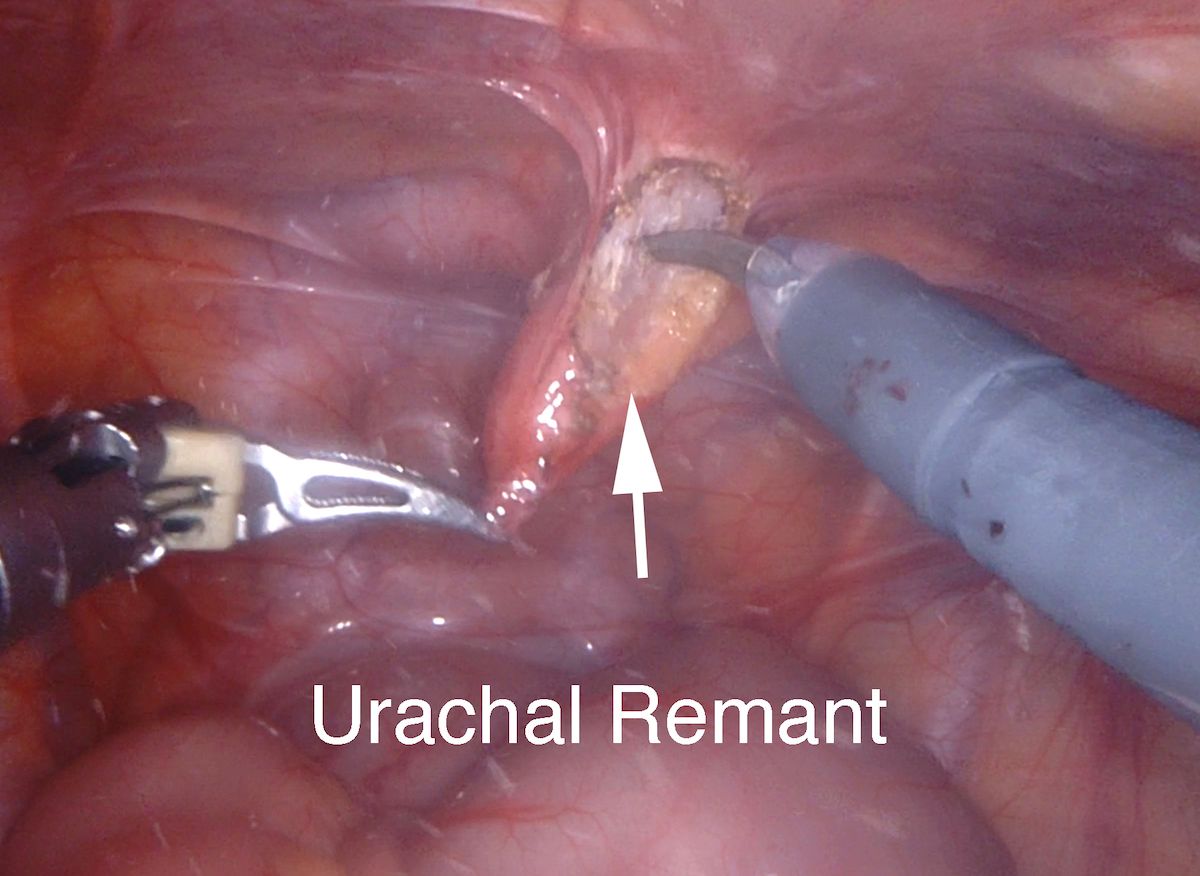
What are our other indications for robotic surgery? A couple times a year, we would remove an infected urachal cyst that we've cooled off with antibiotics. We see a myriad of patients referred to us for an incidental urachal cyst (Figure 6) or urachal remnant, and we leave those patients alone. But the patients who present with a clinical issue—with abdominal pain, a red umbilicus, and/or drainage, we would cool them off with antibiotics and then perform robotic and/or laparoscopic surgery to remove the abnormal urachal remnant. I think either approach is fine. One advantage of the robot is occasionally these urachal remnant cysts can extend into the bladder. So, you'll require a small resection of the dome of the bladder, and you've got the robot available for efficiently suturing the bladder defect in a couple of layers.
Figure 7A
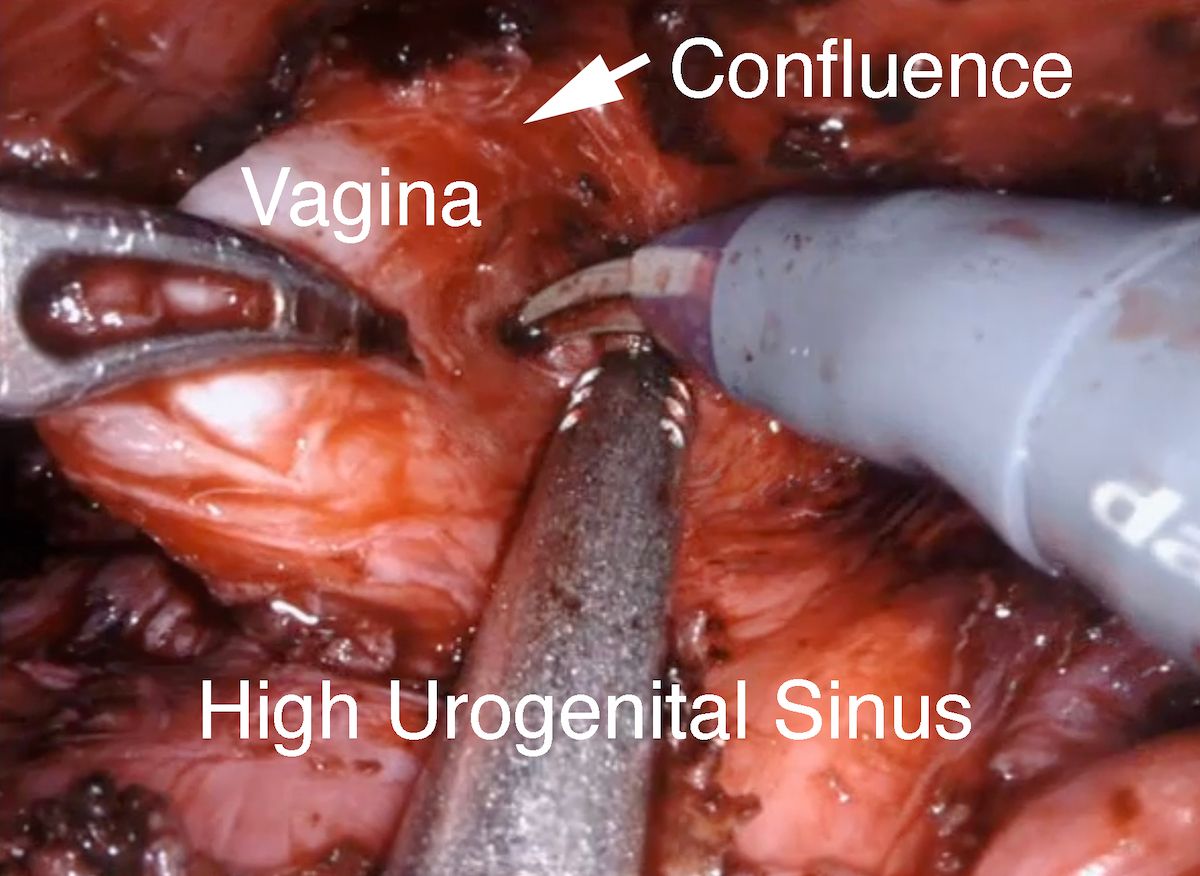
Figure 7B

Finally, where the robot really comes in handy is in patients who have rare pelvic pathology that we would typically do with combined perineal abdominal approach. Examples I would give would be complex high urogenital sinus with a high confluence (Figures 7A and B) patient who have a large prostatic utricle or the rare patient with a rectal duplication (Figure 8). These are relative rare congenital anomalies, but the visualization of the robot deep in the pelvis, and the ability to flip the camera up and down, to precisely dissect in the pelvis and to suture in the pelvis, in a small space—in babies and/or teenagers—is really a spectacular advance.
Figure 8
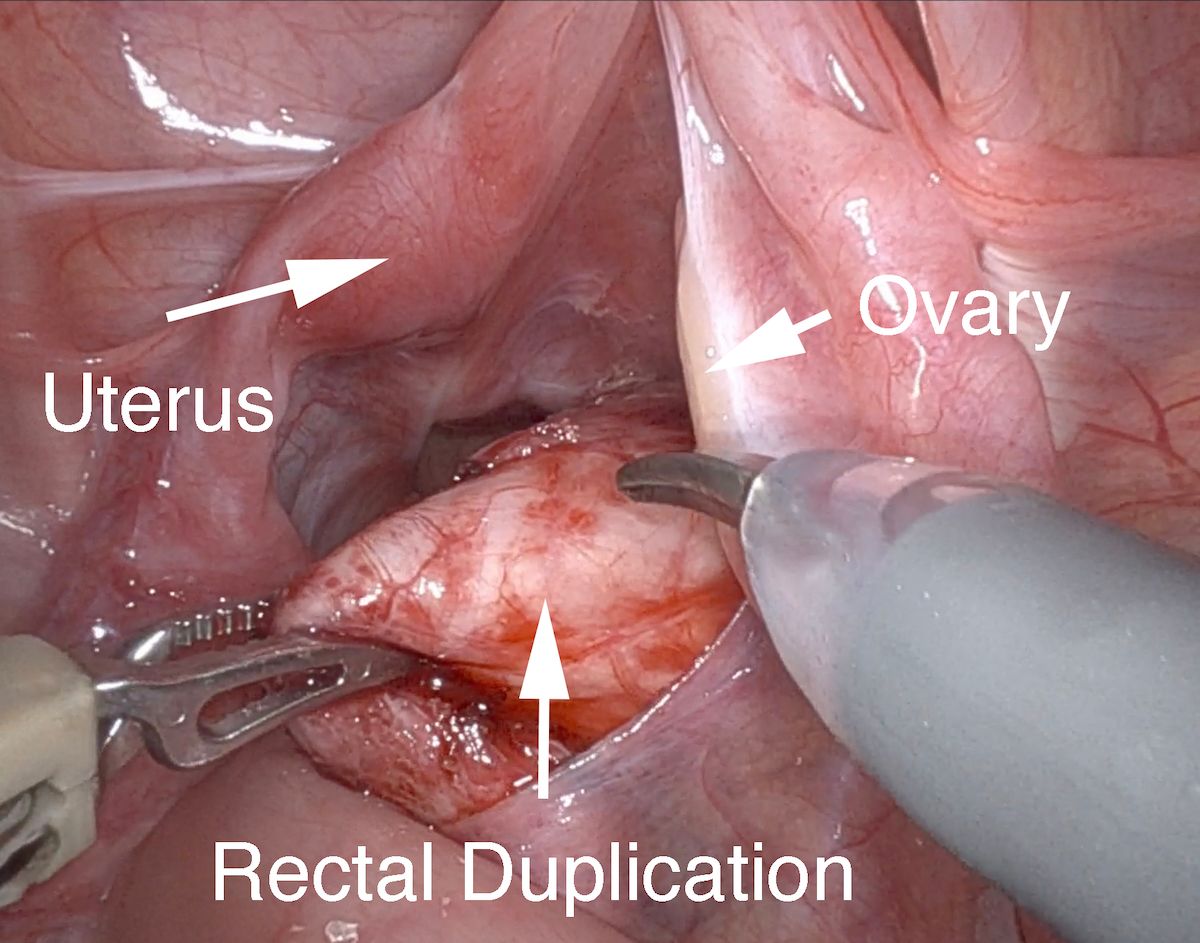
To summarize, we're big advocates for robotic pyeloplasty; we would give that an "A," we would give pelvic surgery, although very rare indications such as separating the confluence of the vagina in a high urogenital sinus, we would also give that an "A." For other things that are relatively rare—urachal remnants, I would give a "B" or "B+," with an overuse for incidental found urachal remnant of sonogram. For patients who have primary ureteral reflux, we would give that robotic surgery a "C" mostly because we don't think that the indications and the success rate are equal to open surgery.
REFERENCE
1. Wang MK, Li Y, Selekman RE, Gaither T, Arnhym A, Baskin LS. Scar acceptance after pediatric urologic surgery. J Pediatr Urol. 2018;14(2):175.e1-175.e6. doi:10.1016/j.jpurol.2017.11.018
Newsletter
Stay current with the latest urology news and practice-changing insights — sign up now for the essential updates every urologist needs.
Pediatric urinary microbiome composition is associated with recurrent UTI
















