Feature
Article
Urology Times Journal
Fertility preservation in patients with testicular cancer
Author(s):
"Full discussion of the various fertility preservation options and an understanding of the fertility implications of the various treatment modalities must be understood by patients for them to make optimal decisions for their reproductive futures," write the authors.
Brooks is a urology resident at Main Line Health in Philadelphia, Pennsylvania. Piraino is an andrology fellow at Mayo Clinic in Rochester, Minnesota. Helo is an assistant professor of urology at Mayo Clinic in Rochester, Minnesota.
Anthony Brooks, MD

Testicular cancer is the most common malignancy in men during their prime reproductive years.1 Oncologic outcomes are excellent, with a 5-year survival rate of more than 95% for most patients, making future fertility an important and often underappreciated aspect of their care.2 Providers should be prepared to counsel patients prior to treatment and throughout the cancer survivorship process.
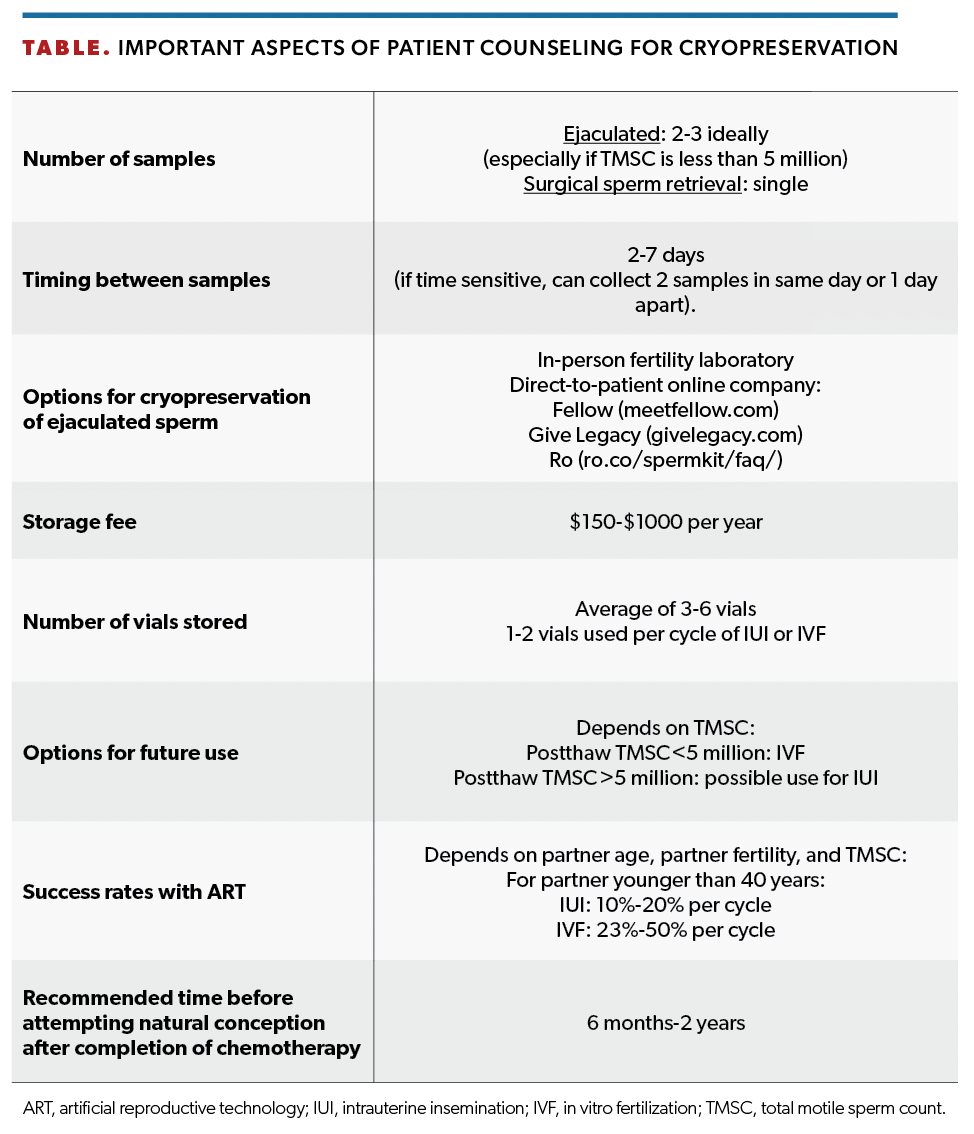
Although American Urological Association and National Comprehensive Cancer Network guidelines advocate for sperm banking, potential barriers include underreferral, cost, access to a laboratory that can perform cryopreservation, and urgent need to begin chemotherapy. Fertility preservation should be offered to all men with a new diagnosis of testicular cancer regardless of age. Assumptions regarding future fertility plans based on a patient’s age, relationship status, or previous paternity may fail to capture all men who desire cryopreservation. Sperm banking is the most used method of cryopreservation because of its widespread availability,
Javier Piraino, DO

cost-effectiveness, and efficacy.3 In recent years, a number of direct-to-patient companies that offer mail-in cryopreservation have surfaced, including Fellow, Give Legacy, and Ro. For patients who do not have access to cryopreservation services locally, this offers convenience in a timely manner. Fellow also offers test kits that providers can stock in their office for patients who need to urgently start chemotherapy.
For men unable to provide a sample, options include a postejaculatory urine specimen for men with retrograde ejaculation, penile vibratory stimulation, or electroejaculation for men with spinal cord injury.4 Finally, in men for whom nonoperative management is not feasible, surgical sperm retrieval with percutaneous aspiration of the epididymis, testicular sperm aspiration, or testicular sperm extraction (TESE) can be performed at the time of radical orchiectomy in either the ipsilateral or contralateral testicle to the cancerous lesion with little added morbidity.5
Sevann Helo, MD

Even prior to treatment, semen abnormalities are commonly affected by direct parenchymal damage as well as correlative causes such as cryptorchidism, which increases the risk of both testicular cancer and infertility.6,7 Other causes for worsened semen parameters in men with testicular cancer include the effects of elevated α-fetoprotein or β–human chorionic gonadotropin on the hypothalamic-pituitary-gonadal axis as well as sequelae of elevated systemic inflammation, temperature, and oxidative stress.8-10 Patients should receive a semen analysis report with their cryopreserved sample that includes the concentration, motility, and volume. A postthaw total motile sperm count (calculated by multiplying the concentration, motility, and volume) greater than 5 to 10 million may allow use of the cryopreserved sample for intrauterine insemination; otherwise, it will need to be used for in vitro fertilization. As a general rule, the freeze-thaw process will cause motility to decline by 25% to 50%.
Beyond initial damage from the cancer, each therapeutic method of treatment causes further insult to fertility. Radical orchiectomy, the first intervention and mainstay of treatment, has been shown to decrease several semen parameters, including total sperm count.11 Even when the contralateral testicle is apparently normal, semen parameters are impaired after orchiectomy in up to 85% of men, with 9% of men developing azoospermia.11 In carefully selected patients, such as patients with bilateral testicular tumors or with a solitary testicle, partial orchiectomy when appropriate from an oncologic standpoint may be a way to mitigate effects on fertility.12
Chemotherapy has well-recognized gonadotoxic effects. In particular, platinum-based chemotherapy agents cisplatin and carboplatin, which are commonly used for testis cancer, pose an intermediate risk for permanent azoospermia.6 Fortunately, the majority of patients recover spermatogenesis after completion of chemotherapy, although it takes most men several years for this to occur and the amount of time required to recover spermatogenesis increases in a dose-dependent fashion with the number of cycles of chemotherapy.13 Other commonly used agents bleomycin and etoposide are lower risk and tend to cause only a temporary reduction in spermatogenesis.6 The alkylating agents cyclophosphamide and ifosfamide pose the highest risk of permanent azoospermia and cause persistent azoospermia in 25% of men 5 years after treatment.14
Radiation also affects testicular function in a dose-dependent manner.15 With appropriate gonadal shielding, radiation doses to the testicle can be as low as 0.28% of the treatment dose, limiting the gonadotoxic effects to the testis during radiation of the retroperitoneum.16 However, in men receiving radiation to the testicle after partial orchiectomy, there will be an expectantly high rate of irreversible azoospermia.17 Compared with germinal epithelium, Leydig cells are more resistant to radiation exposure, but 15% to 25% of men receiving testicular radiation will ultimately need testosterone replacement, and these men should be monitored appropriately.6,17 Additionally, the radiation from surveillance imaging should not be overlooked and established protocols should be followed to limit unnecessary radiation exposure.6 Retroperitoneal pelvic lymph node dissection (RPLND) is performed as a primary or salvage treatment and places patients at risk for anejaculation or retrograde ejaculation due to disruption of the sympathetic nerves or hypogastric plexus responsible for emission and ejaculation.18 When oncologically amenable, modern nerve-sparing RPLND techniques result in less than 10% of patients experiencing significant ejaculatory complications.18
In addition to the physical effects of testicular cancer and its subsequent treatments, men commonly experience symptoms of sexual dysfunction. Up to 40% of men have erectile dysfunction after treatment (regardless of treatment modality), and similar numbers of men report decreased libido and decreased sexual activity.19,20 A majority of men report some degree of ejaculatory complaint and decreased overall sexual satisfaction.20 In findings from one study, penile duplex ultrasound on patients with erectile dysfunction 12 months after treatment revealed all patients to have normal hemodynamics, supporting a psychogenic etiology to their symptoms and emphasizing the importance of awareness and appropriate nonpharmacologic therapy to address these common complaints.21
Ideally, all patients would cryopreserve prior to treatment, but recognizing that some sperm is better than no sperm, we would advocate the option to cryopreserve at any step in the treatment process. Although many patients will have recovery of spermatogenesis after treatment with chemotherapy, it is difficult to predict outcomes for any specific patient. Microdissection TESE (mTESE) and subsequent intracytoplasmic sperm injection have been established as the gold standard for men with azoospermia to achieve biologic paternity.22 In findings from several studies, sperm has been successfully retrieved in approximately 40% of men with azoospermia after chemotherapy by using mTESE.23 Thus, mTESE can be an effective treatment option for men with persistent azoospermia after chemotherapy but is clearly inferior to up-front cryopreservation prior to gonadotoxic treatment. It is important to note that successful paternity can be achieved in patients with testicular cancer regardless of treatment modality. Results from one study found that of men attempting conception after treatment, paternity was achieved naturally in 77%, with rates ranging from 85% in men after orchiectomy followed by surveillance to as low as 67% in men after chemotherapy plus radiation.24
Even after recovery of spermatogenesis, the quality of sperm produced is not certain, with additional risk of sperm aneuploidies and DNA fragmentation for months after treatment.25 Most experts advocate waiting 6 months to 2 years after chemotherapy or radiation prior to attempting to conceive. Conversely, there is also a risk of affecting sperm quality with cryopreservation, but there is no evidence that this leads to adverse pregnancy outcomes or congenital malformations.6
In conclusion, fertility preservation in testicular cancer is a complex and underused process. Early discussion of options is essential for management. Sperm cryopreservation prior to undergoing treatment remains the most effective and cost-effective strategy for fertility preservation and should be emphasized as such. Full discussion of the various fertility preservation options and an understanding of the fertility implications of the various treatment modalities must be understood by patients for them to make optimal decisions for their reproductive futures.
References
1. Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics, 2023. CA Cancer J Clin. 2023;73(1):17-48. doi:10.3322/caac.21763
2. Cancer stat facts: testicular cancer. National Cancer Institute. Accessed January 23, 2024. http://tinyurl.com/35b8rdhs
3. Gilbert K, Nangia AK, Dupree JM, Smith JF, Mehta A. Fertility preservation for men with testicular cancer: is sperm cryopreservation cost effective in the era of assisted reproductive technology? Urol Oncol. 2018;36(3):92.e1-92.e9. doi:10.1016/j.urolonc.2017.11.002
4. Fode M, Ohl DA, Sønksen J. A step-wise approach to sperm retrieval in men with neurogenic anejaculation. Nat Rev Urol. 2015;12(11):607-616. doi:10.1038/nrurol.2015.241
5. Leung A, Mira J, Hsiao W. Updates on sperm retrieval techniques. Transl Androl Urol. 2014;3(1):94-101. doi:10.3978/j.issn.2223-4683.2014.02.03
6. Parekh NV, Lundy SD, Vij SC. Fertility considerations in men with testicular cancer. Transl Androl Urol. 2020;9(suppl 1):S14-S23. doi:10.21037/tau.2019.08.08
7. Caroppo E, Niederberger C, Elhanbly S, Schoor R, Ross L, D’Amato G. Effect of cryptorchidism and retractile testes on male factor infertility: a multicenter, retrospective, chart review. Fertil Steril. 2005;83(5):1581-1584. doi:10.1016/j.fertnstert.2005.01.088
8. Coward RM, Kovac JR, Smith RP, Lipshultz LI. Fertility preservation in young men treated for malignancies: options for precancer treatment. Sex Med Rev. 2013;1(3):123-134. doi:10.1002/smrj.13
9. Hansen PV, Trykker H, Andersen J, Helkjaer PE. Germ cell function and hormonal status in patients with testicular cancer. Cancer. 1989;64(4):956-961. doi:10.1002/1097-0142(19890815)64:4<956::aid-cncr2820640431>3.0.co;2-3
10. Fankhauser CD, Sander S, Roth L, et al. Systemic inflammatory markers have independent prognostic value in patients with metastatic testicular germ cell tumours undergoing first-line chemotherapy. Br J Cancer. 2018;118(6):825-830. doi:10.1038/bjc.2017.467
11. Petersen PM, Skakkebaek NE, Rørth M, Giwercman A. Semen quality and reproductive hormones before and after orchiectomy in men with testicular cancer. J Urol. 1999;161(3):822-826.
12. Bazzi WM, Raheem OA, Stroup SP, Kane CJ, Derweesh IH, Downs TM. Partial orchiectomy and testis intratubular germ cell neoplasia: world literature review. Urol Ann. 2011;3(3):115-118. doi:10.4103/0974-7796.84948
13. Lampe H, Horwich A, Norman A, Nicholls J, Dearnaley DP. Fertility after chemotherapy for testicular germ cell cancers. J Clin Oncol. 1997;15(1):239-245. doi:10.1200/JCO.1997.15.1.239
14. Green DM, Liu W, Kutteh WH, et al. Cumulative alkylating agent exposure and semen parameters in adult survivors of childhood cancer: a report from the St Jude Lifetime Cohort Study. Lancet Oncol. 2014;15(11):1215-1223. doi:10.1016/S1470-2045(14)70408-5
15. Rowley MJ, Leach DR, Warner GA, Heller CG. Effect of graded doses of ionizing radiation on the human testis. Radiat Res. 1974;59(3):665-678.
16. Singhal MK, Kapoor A, Singh D, et al. Scattered radiation to gonads: role of testicular shielding for para-aortic and homolateral illiac nodal radiotherapy. J Egypt Natl Canc Inst. 2014;26(2):99-101. doi:10.1016/j.jnci.2014.03.002
17.Ory J, Blankstein U, Gonzalez DC, et al. Outcomes of organ-sparing surgery for adult testicular tumors:A systemic review of the literature. BJUI Compass. 2021;2(5):306-321. doi: 10.1002/bco2.77
18. Masterson TA, Cary C, Rice KR, Foster RS. The evolution and technique of nerve-sparing retroperitoneal lymphadenectomy. Urol Clin North Am. 2015;42(3):311-320. doi:10.1016/j.ucl.2015.04.005
19. Wiechno P, Demkow T, Kubiak K, Sadowska M, Kamińska J. The quality of life and hormonal disturbances in testicular cancer survivors in cisplatin era. Eur Urol. 2007;52(5):1448-1454. doi:10.1016/j.eururo.2007.05.012
20.Pühse G, Wachsmuth JU, Kemper S, Husstedt IW, Evers S, Kliesch S. Chronic pain has a negative impact on sexuality in testis cancer survivors. J Androl. 2012;33(5):886-893. doi:10.2164/jandrol.110.012500
21. Tal R, Stember DS, Logmanieh N, Narus J, Mulhall JP. Erectile dysfunction in men treated for testicular cancer. BJU Int. 2014;113(6):907-910. doi:10.1111/bju.12331
22. Meseguer M, Garrido N, Remohí J, et al. Testicular sperm extraction (TESE) and ICSI in patients with permanent azoospermia after chemotherapy. Hum Reprod. 2003;18(6):1281-1285. doi:10.1093/humrep/deg260
23. Hsiao W, Stahl PJ, Osterberg EC, et al. Successful treatment of postchemotherapy azoospermia with microsurgical testicular sperm extraction: the Weill Cornell experience. J Clin Oncol. 2011;29(12):1607-1611. doi:10.1200/JCO.2010.33.7808
24. Huddart RA, Norman A, Moynihan C, et al. Fertility, gonadal and sexual function in survivors of testicular cancer. Br J Cancer. 2005;93(2):200-207. doi:10.1038/sj.bjc.6602677
25. Rives N, Walschaerts M, Setif V, et al. Sperm aneuploidy after testicular cancer treatment: data from a prospective multicenter study performed within the French Centre d’Étude et de Conservation des Oeufs et du Sperme network. Fertil Steril. 2017;107(3):580-588.e1. doi:10.1016/j.fertnstert.2016.11.015

Newsletter
Stay current with the latest urology news and practice-changing insights — sign up now for the essential updates every urologist needs.