
Solaris Health
Latest Content

“[There’s] a lot going on in bladder cancer in the non–muscle invasive, muscle-invasive space, as well as in some of the biomarkers, which is exciting and will definitely have a huge impact on the management of your patients," says Jason M. Hafron, MD, CMO.

“As we move through 2025, I think we're going to see more and more expansion of new ideas, new isotopes, and possibly improvement in PET imaging for the future,” says Jason M. Hafron, MD, CMO.

Arpeet Shah, MD, highlights the shift toward precision medicine, ongoing work force challenges, the integration of AI, and more.

"Things that were typically used to recruit younger physicians need to change because those aren't their priorities anymore," says Kari Bailey, MD.

"It's a little tedious to find these patients, but it's really critical. Otherwise, you're not going to get reimbursed for these therapies," says Jason Hafron, MD.

“The guidelines have changed. They used to be called third-line therapies, and they're no longer quote "third-line" anymore, based on the new guidelines that have come out,” says Kari Bailey, MD.

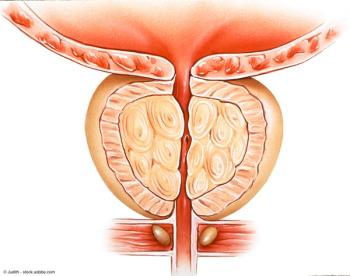
The panel concludes by addressing unmet needs in prostate cancer management, with a particular focus on improving risk stratification methods.

The panel explores promising biomarker research that has the potential to significantly impact patient care in prostate cancer.

Prostate cancer specialists share their insights on anticipated future advancements that could significantly influence prostate cancer management strategies.

The key opinion leaders explore strategies for integrating newly available diagnostic tests into the existing treatment paradigm and patient journey.

The panel examines the significance of biomarkers in assessing therapy outcomes for prostate cancer patients, while also exploring the concept of absolute benefit in metastasis risk when adding androgen deprivation therapy (ADT) to radiation therapy for newly diagnosed cases.

The panel explores the role of biomarkers in monitoring disease progression for prostate cancer patients on active surveillance, discussing how these tests aid in detecting changes that may warrant intervention.

The panel examines the challenges associated with effectively interpreting and applying biomarker test results in prostate cancer management and treatment decision-making.

The key opinion leaders explore various treatment approaches for prostate cancer, including surgery, radiation, and hormone therapy, explaining how biomarker results influence their treatment choices. They also detail the specific criteria they use to select between treatment options based on biomarker testing outcomes.

The panelists examine the challenges and limitations they've faced when using the Gleason score for risk assessment in prostate cancer patients, while also highlighting how biomarker testing has informed and guided their treatment strategies.

Medical oncologists explore risk stratification strategies for newly diagnosed patients with prostate cancer, emphasizing the significant role of the Gleason score in diagnosis and prognosis.

The key opinion leaders explore risk factors for prostate cancer, detailing both general risk groups and high-risk populations more susceptible to developing the disease.

Prostate cancer management experts share their clinical insights on selecting appropriate serum, urine, and/or tissue biomarkers, highlighting specific scenarios that warrant each type of test.

The panel emphasizes the crucial need for swift biomarker and genetic testing to facilitate timely and effective patient care in prostate cancer management.

The key opinion leaders explore the challenges and limitations associated with using prostate-specific antigen (PSA) as a biomarker for prostate cancer detection and monitoring.

The panel of experts in prostate cancer offers a comprehensive overview of prostate cancer diagnosis, emphasizing the role of prostate-specific antigen (PSA) testing in screening for the disease.

A novel co-formulation of bremelanotide and a PDE5 inhibitor allows the treatment to be administered to patients via a single injection.

"From a learning curve standpoint, there's not much to learn. It tends to be fairly quick in terms of your ability to do the procedure," says Matthew E. Sterling, MD.

"I think it's important that they go visit someone that does them. Go to the operating room, see it in person," says Matthew E. Sterling, MD.

"Some of it actually is self-selecting because people are hearing about it more and come in asking about it first," says Brian Friel, MD.

"The learning curve is fairly quick; you can pick this up pretty easily vs some of the other prostate procedures that can take a little bit more time to learn how to use," says Matthew E. Sterling, MD.
"The limitation of [TURP] is you're shaving out prostate tissue in a layer at a time, and you stop when you think you're deep enough, whereas with an Aquablation, you map all that out ahead of time," says Brian Friel, MD.

"At MIU, we host many ancillary services, including complete ultrasound services, UroCuff, urodynamics, PTNS [percutaneous tibial nerve stimulation], full laboratory and pathology services, Xofigo [radium-223]," says Jason M. Hafron, MD.

Dr. Shawn Zimberg and Dr. Dean Laganosky discuss the BioProtect Balloon Transplant System, a rectal spacer for use in prostate cancer radiation.
