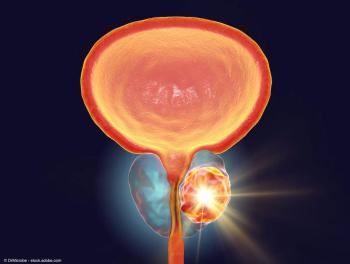
PSMA-PET imaging has successfully disrupted the prostate cancer paradigm and experts agree that unleashing the full potential of this breakthrough requires a multidisciplinary approach.
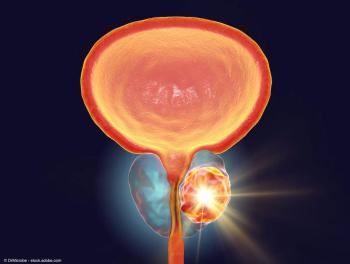
PSMA-PET imaging has successfully disrupted the prostate cancer paradigm and experts agree that unleashing the full potential of this breakthrough requires a multidisciplinary approach.

“I think that having the clinical context such as the PSA, the Gleason score, the other features that assess the aggressiveness of the disease can really help with some of these subtle findings that can be found on PET imaging,” says Daniel Spratt, MD.

Daniel Spratt, MD, highlights the evolving paradigm of PET-based imaging agents in prostate cancer, with a focus on the impact of PSMA-PET imaging.

Jaideep S. Sohi, MD, discusses the challenges with the use of conventional imaging in prostate cancer and how PSMA-PET alleviates these issues.

In this video, Jaideep S. Sohi, MD, explains factors to consider regarding the timing of re-imaging with PSMA-PET in patients with prostate cancer.

In this video, Jaideep S. Sohi, MD, explains how the expanded information provided by PSMA-PET imaging allows physicians to more accurately tailor treatment plans for patients.

Jaideep S. Sohi, MD, shares his vision for the future of PSMA-PET imaging in prostate cancer.
“If approved by the FDA, this new product will have a significant impact on prostate cancer patients, physicians, and their caregivers by helping to eliminate the inequity of access to PSMA-PET agents, and increase the ability to accurately diagnose cancer early, reducing the cost of care, and increasing the probability of patients’ survival," says Mike Crosby.

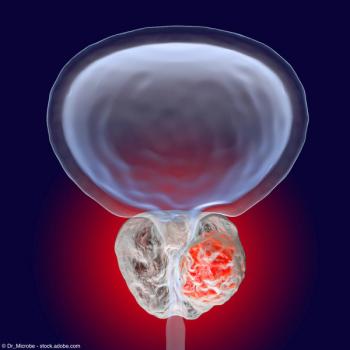
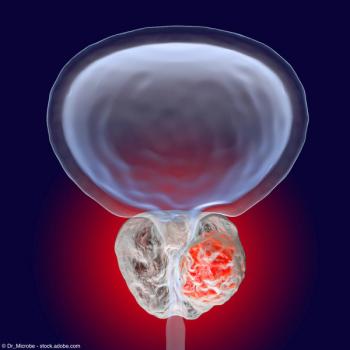
Patients with high-risk disease were shown to have a significantly higher mean value of SUVmax compared with patients with low-risk disease (23.5 ± 13.2 vs 10.6 ± 5.4; P < 0.05).

“And certainly, while most of these studies are ongoing, the initial data looks promising to say that there may be a role for a PSMA next-generation imaging in the decision for the appropriateness for active surveillance,” says Brian T. Helfand, MD, PhD.

“I think this is really playing a role in the decision for where we're localizing our radiation therapies as well as the addition of ADT plus an androgen receptor pathway inhibitor, ARPI, and the duration of these therapies,” says Brian T. Helfand, MD, PhD.

"Understanding that biology of that tumor and/or combining or using multiple radiotracers, either simultaneously or in sequence, may really be exciting to identify where those tumors are located," says Brian T. Helfand, MD, PhD.
“I think the use and the appropriateness of these agents along the patient journey is also coming into question,” says Brian T. Helfand, MD, PhD.

The median PFS with PSMA PET/CT-guided MDT was 33.2 months, vs 13.8 months with choline PET/CT-guided MDT.

"The radiologist more than ever has to be part of the care team," says Phillip H. Kuo, MD, PhD, FACR.
“Nowadays with PET, it's not perfect, but even with a PSA less than 1 ng/mL, we can detect the site of recurrence about 2/3 of the time,” says Bridget Koontz, MD.

“The majority (76%) of patients not yet meeting the Phoenix criteria did have PSMA-avid lesions on PSMA-PET, suggesting [prostate cancer] recurrence," says Evelien J E van Altena.
“And you look at most of the trials that were done in this space, about 2/3 of time, over 60% of time, management was changed based on a PET scan,” says Jason Hafron, MD.

“Time will tell as we move forward, but it has allowed us to use MDT, with or without ADT and ARPIs, to potentially look at hormone-free treatments,” says Jason M. Hafron, MD, CMO.

"But as you get out of expert centers and academic sites that did it for years under research protocols, the level of the quality of the reads decreases," says Jeremie Calais, MD, PhD.

“It encompasses and contains the miTNM, PROMISE, PRIMARY, RECIP, PSMA-RADS, and E-PSMA concept and criteria all together,” says Jeremie Calais, MD, PhD.

“It encompasses and contains the miTNM, PROMISE, PRIMARY, RECIP, PSMA-RADS, and E-PSMA concept and criteria all together,” says Jeremie Calais, MD, PhD.

The investigators found a positive correlation between PSA levels and SUVmax.

“In some ways, it can be used to help if you want to get a biopsy to prove or confirm—it can be used to help detect in that range, too,” says Michael S. Cookson, MD, MMHC, FACS.