Article
Integrating video visits into urologic training
Author(s):
"Now is the time for programs to leverage their existing telehealth platforms and practices for trainee education while continuing to serve patients," the authors write.
In recent years, telemedicine has gained traction across different facets of health care, including urology.1 However, the COVID-19 pandemic created an urgent need for virtual care never experienced before. Michigan Medicine in Ann Arbor, for example, was conducting approximately 40,000 video visits per month in May 2020, of which 1100 were through the urology department.2
Although in-person care resumed in all Michigan Medicine urology clinics in July 2020, approximately 20% of patient visits since then have been virtual. The widespread use of telehealth leads experts to believe that a portion of all urologic care will remain virtual even beyond the pandemic.
COVID-19 cases are again surging, with more than 100,000 new cases daily in the United States. Limitations on in-person care may be required again in the near future to address finite hospital and clinic capacities. Now is the time for programs to leverage their existing telehealth platforms and practices for trainee education while continuing to serve patients. To help with this, a workflow was created for integrating learners into video visits that can be adopted and optimized to fit different clinic and institutional needs (Figure).
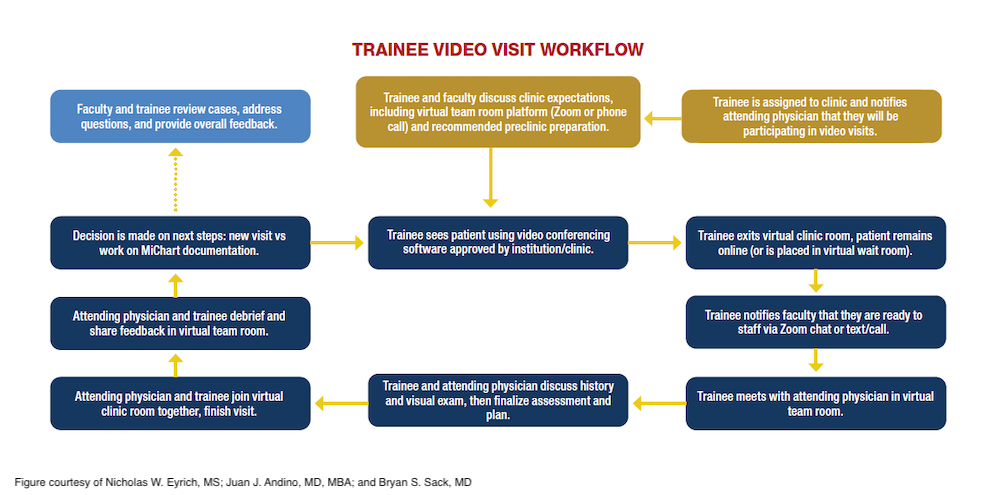
Between April 27 and May 15, 2020, a pilot program of 50 resident and medical student video visits was conducted through Michigan Medicine's Department of Urology, including adult and pediatric subspecialties. Written, qualitative feedback was obtained after each virtual clinic. Lessons learned were condensed to the following main workflow components critical for successful patient care and optimal trainee learning:
- Prior to virtual clinic, the assigned trainee should touch base with the attending physician to discuss expectations and their platform of choice for a virtual team room (e.g., phone, Zoom, or other video conferencing software).
- During the video visit, the trainee sees the patient on their own in a virtual clinic room, then virtually exits after asking the patient to remain. Alternatively, some platforms allow patients to be relocated to a waiting room.
- The trainee then contacts the attending to staff in the virtual team room that was established previously.
- Once an assessment and plan have been discussed, the attending and the trainee enter the virtual clinic room for shared decision-making and conclusion of the video visit with the patient.
- The trainee and attending then debrief in the virtual team room with relevant teaching points, feedback, and next steps for that day’s clinic.
Following these pilot video visits, faculty were asked to provide comments based on their experience. Regarding the educational utility of video visits, one faculty member said, “I thought the learning opportunities were excellent. I think the opportunity to learn from attendings virtually may even be better than in a physical clinic because there are fewer distractions.”
Similarly, another urologist reported, “The structured format might provide more face-to-face time with attendings than students may otherwise have in a busy clinic.”
As a result of these efforts, this workflow has been disseminated across Michigan Medicine for medical student and resident education to ensure that trainees are able to deliver virtual care.
This work lays the foundation for trainee integration into virtual clinics to allow for real-world learning and early exposure to delivering care via telehealth. More robust and objective evaluations are necessary to move beyond proof of concept and ensure that appropriate educational milestones and standards are upheld. This framework helps address challenges related to the ongoing COVID-19 pandemic while preparing the workforce of the future.
Eyrich is a fourth-year medical student, Andino is a urology resident, and Sack is an assistant professor of urology at the University of Michigan, Ann Arbor.
Acknowledgements
Michael S. Sessine, BS; and Emma C. Bethel, BA, of the University of Michigan Medical School in Ann Arbor, MI helped organize and coordinate this pilot project while participating in video visit as students.
Chad Ellimoottil, MD, MS; Courtney Streur, MD; Todd Morgan, MD; Miriam Hadj-Moussa, MD; Jeffrey Montgomery, MD; Anne Pelletier-Cameron, MD; and Jim Dupree, MD, volunteered their clinic time for this pilot at Michigan Medicine.
References
1. Castaneda P, Ellimoottil C. Current use of telehealth in urology: a review. World J Urol. 2020;38(10):2377-2384. doi:10.1007/s00345-019-02882-9
2. Caring at a distance: telehealth and the COVID-19 pandemic. News release. University of Michigan Institute for Healthcare Policy & Innovation. April 27, 2020. Accessed November 6, 2020. https://bit.ly/32kJdyS
Suggested reading
1. Andino JJ, Lingaya MA, Daignault-Newton S, Shah PK, Ellimoottil C. Video visits as a substitute for urological clinic visits. Urology. 2020;144:46-51. doi:10.1016/j.urology.2020.05.080
2. Gadzinski AJ, Ellimoottil C. Telehealth in urology after the COVID-19 pandemic. Nat Rev Urol. 2020;17(7):363-364. doi:10.1038/s41585-020-0336-6
3. Ellimoottil C. What will urology look like in 2035? Nat Rev Urol. 2019;16(11):635-636. doi:10.1038/s41585-019-0239-6
Newsletter
Stay current with the latest urology news and practice-changing insights — sign up now for the essential updates every urologist needs.