
"To me, the most compelling outcome is really the quality-of-life outcomes. General quality of life as well as emotional quality of life improved in the intervention group significantly," says Jill M. Hamilton Reeves, PhD, RD, CSO.

"To me, the most compelling outcome is really the quality-of-life outcomes. General quality of life as well as emotional quality of life improved in the intervention group significantly," says Jill M. Hamilton Reeves, PhD, RD, CSO.
“We found that the SAPS is associated with higher intrarenal pressure and flow rate when compared to automated pumps," said Lucas B. Vergamini, MD.

"The point is healthy, adaptive changes that are sustainable, that you can keep off, because we don't want that rebound/regain," says Jill M. Hamilton-Reeves, PhD, RD, CSO.


"The biggest finding was that the guys lost the weight. They lost 5.5% of their body weight," says Jill M. Hamilton Reeves, PhD, RD, CSO.

"We had interest in trying to look at mechanisms and seeing if the obvious question is, well, if obesity is associated with progressing cancer, can we disrupt that link if we help men lose weight in a healthy way," says Jill Hamilton Reeves, PhD, RD, CSO.

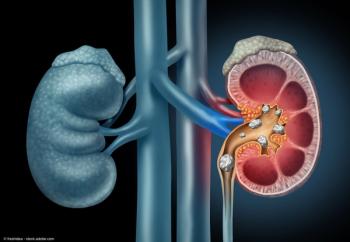
The patient presented with a large right renal mass who elected for right radical nephrectomy with possible inferior vena cava.

Moben Mirza, MD, FACS, discusses the need to move toward an optimal number of urology residency applications for both the individual applicants and the residency programs.

“It was overall received very positively by applicants and programs,” says Moben Mirza MD.

“There’s always going to be some criticism…but I think we can see what needs to improve and move toward a system that works well for everyone,” says Moben Mirza MD.

“Number 1 to me is going to be an applicant who comes in ready to avail all the opportunity that will be afforded to them during their residency,” says Moben Mirza MD.
“We have helped developed policies at the national level as far as parental leave for residents and fellows, helping to streamline a lot of that process with the American Board of Urology,” says Daniel Igel, MD.

“You do need to be a little bit careful because of the risk of priapism,” says Joshua A. Broghammer, MD.
“I think that we’re going to see more and more advances in how we use mpMRI from a pre-treatment planning perspective,” William P. Parker, MD.

William P. Parker, MD, discusses the initial use of MRI and emergence of multiparametric MRI in the prostate cancer paradigm.
Joshua A. Broghammer, MD, discusses the development and use of intracavernosal injections for the treatment of patients with erectile dysfunction.
“From a screening perspective, mpMRI really has changed how we evaluate men at risk for prostate cancer. It has improved the selection of men for biopsy and certainly improved our diagnostic rates,” says William P. Parker, MD.
Joshua A. Broghammer, MD, discusses the use of penile implants in the field of urology, detailing both the semi-rigid and inflatable penile prostheses.

William P. Parker, MD, highlights 3 areas in which he thinks PSMA-PET imaging is going to be explored further in prostate cancer.
There are 2 FDA-approved PSMA-PET imaging agents: Gallium 68 PSMA-11 (Ga 68 PSMA-11) and piflufolastat F 18.

In this interview, William P. Parker, MD, highlights the development of PSMA-PET imaging in prostate cancer, FDA-approved PSMA-PET agents, and the next steps with this disruptive technique.
“PSMA-PET imaging is something that from a clinical practice perspective is rapidly changing and evolving the field of prostate cancer,” says William P. Parker, MD.

“The leadership has really driven this program to be one of the best in the country,” says Casey Kowalik, MD.

“There is so much support and so much advocacy to work and create an equitable culture for women in this historically male-dominated field,” says Casey Kowalik, MD.
Danica May, MD, discusses positive feedback she has received from participants in the KU Department of Urology rotation.
“We still need better representation from the AUA national level on down to the section meeting. There is a positive push for that, but things are still in process,” says Danica May, MD.
“It’s always fun getting to interact with people from different programs and different areas and we want to make them feel as welcome as possible,” says Danica May, MD.

For the essay contest, urology residents and fellows were asked to predict the future of the specialty from their point of view.

On this podcast, Lieutenant Colonel Matthew Banti, MD, FACS, a recent graduate of the Urologic Oncology fellowship at the University of Kansas Health System, is interviewed about his career journey as a urologist in the United States Army.

A recent study published in Urology described how American Urological Association–accredited urological residency training programs are organized in terms of clinical exposure and teaching of their residents.