CAPTAIN trial highlights early advantages of TULSA vs prostatectomy
TULSA patients were treated and discharged the same day.
Episodes in this series

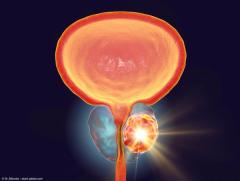
In this video, recorded at the 2025 Society of Urologic Oncology Annual Meeting in Phoenix, Arizona, Geoffrey Sonn, MD, an associate professor of urology and, by courtesy, of radiology (body MRI) at Stanford University in Stanford, California, discusses the rationale, design, and early findings of the CAPTAIN trial, the first randomized controlled study comparing transurethral ultrasound ablation (TULSA) with radical prostatectomy for men with intermediate-risk prostate cancer. He explains that although multiple focal and whole-gland ablative technologies exist, none have previously been tested head-to-head against surgery in a randomized format. As a result, clinicians have relied primarily on case series, limiting the ability to draw definitive conclusions about comparative cancer control and adverse event profiles. CAPTAIN was created to directly address this gap, and its successful completion of target enrollment is a major milestone in a field where randomization has historically been difficult.
The trial enrolled men with grade group 2 or 3 prostate cancer—the population most commonly treated surgically today. Participants were randomly assigned 2:1, with 2 patients assigned to TULSA for every 1 assigned to prostatectomy. TULSA could be administered as whole-gland or partial-gland ablation, provided at least half of the prostate was treated. The study’s primary end points include 1-year functional outcomes—pad-free continence and preservation of sexual function in men with good baseline function—and 3-year oncologic outcomes such as need for salvage therapy, metastasis, and cancer-specific end points. Long-term results are still pending, as the final participant was treated only months ago.
At this meeting, the team presented peri-procedural and early recovery findings. As expected, TULSA demonstrated markedly lower blood loss, since the procedure causes virtually none. Hospital stay was also shorter: TULSA patients were treated and discharged the same day, whereas prostatectomy patients typically stayed just over 1 night. Pain scores favored TULSA during the first postoperative week, though differences disappeared by weeks 3 to 4. Patient-reported overall health was better during the first month for the TULSA group and, although the gap narrowed over time, it did not reverse.
Sonn emphasizes that although short-term recovery appears better with TULSA, the critical questions—cancer control, urinary function, and sexual outcomes—await future results.
Newsletter
Stay current with the latest urology news and practice-changing insights — sign up now for the essential updates every urologist needs.