
Steven A. Kaplan, MD, frames the greatest value of ProVee not as competition with other procedures, but as a compelling alternative to chronic medical therapy.

Steven A. Kaplan, MD, frames the greatest value of ProVee not as competition with other procedures, but as a compelling alternative to chronic medical therapy.

Steven A. Kaplan, MD, emphasizes that ProVee is well suited for office-based or ambulatory settings and is designed to be performed under local anesthesia

Mechanistically, Kaplan emphasizes that ProVee’s key differentiator is not simply that it is an expanding urethral device, but that it belongs to a new class of flexible, catheter-like technologies.

"Suctioning technology for mini-PCNL is an improvement on relying on passive outflow," says Mantu Gupta, MD.

John P. Sfakianos, MD, discusses the significance of urine-based biomarkers for intermediate-risk patients and outlines key findings from the STRATA study.
In his latest YouTube masterclass, Dr. Ash Tewari shares his groundbreaking approach to nerve sparing prostate surgery, shedding light on the anatomy, surgical techniques, and innovations that make it possible.

Catch up on exclusive videos you may have missed from the first half of the year.
No device- or procedure-related serious AEs were observed through 12 months across the entire study population
Matthew D. Galsky, MD, discusses how urologists should approach patient selection for perioperative durvalumab plus chemotherapy based on eligibility criteria for the NIAGARA trial.
"This is another tool in our armamentarium to treat muscle-invasive bladder cancer and represents an advance compared to where we've been over the past few decades," says Matthew D. Galsky, MD.

“High risk, non–muscle invasive bladder cancer carries a significant risk of recurrence and progression. This emphasizes the need for careful patient selection, especially when we are considering bladder-sparing approaches," says Neeraja Tillu, MD.

“Identification of significant predictors [of upstaging] has improved our pre-op counseling," says Neeraja Tillu, MD.

As the year comes to a close, we revisit some of this year’s top video content from Urology Times.


“So, the concept behind delivering something orally in a spray is to hopefully avoid the whole GI effect and get faster absorption,” says Steven A. Kaplan, MD.

"It's the creating of things for me that drives me. Even my wife tells me, 'You are most happy when you're creating new things,' " says Steven A. Kaplan, MD.
“We will do exactly what we have done in terms of prototype of our processes, our tools, our design, and how we follow these patients up, and expand this from 10,000 men in less than 2 years to 1 million men in next 10 years,” says Ashutosh K. Tewari, MD.

Aspargo plans to file a new drug application with the FDA to support regulatory approval of ASP-001 for erectile dysfunction in the United States.

"We can individualize the access and the way we do the operation based on the patient's characteristics, and that hasn't happened in a very long time," says Ketan K. Badani, MD.

Kyrollis Attalla, MD, remarks on emerging imaging technologies for patients with prostate cancer and the growing pool of candidates for focal therapy.

An expert on prostate cancer discusses how fusion-guided biopsy can help determine patient eligibility for focal therapy.

A urologic oncologist discusses how MRI- or fusion-guided biopsies have helped overcome the limitations of traditional prostate biopsies.

A urologic oncologist discusses how MRI- or fusion-guided biopsies have helped overcome the limitations of traditional prostate biopsies.

Kyrollis Attalla, MD, shares his approach to imaging and biopsy in the diagnosis of prostate cancer and discusses the benefit of a good biopsy followed by appropriate imaging at initial diagnosis.

"Somebody once gave me a saying: the 3 things that make a person happy every day are somewhere to go, someone to love, and something to look forward to. I have all 3 of them," says Steven A. Kaplan, MD.
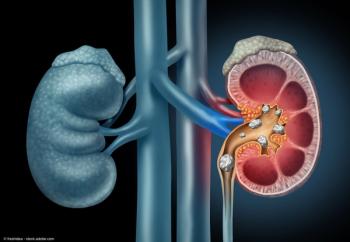
"We found that as we got better and better at doing it, the majority of patients now can go home in this fashion. They can go home the day of the procedure with nothing in them," says Mantu Gupta, MD.

"Even at my stage of career, most people are retiring, and I've never been busier or had more fun," says Steven A. Kaplan, MD.
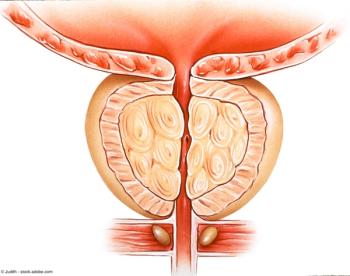
“Our results demonstrated that treatment with [the] Optilume BPH procedure resulted in significant symptom relief while still preserving erectile and ejaculatory function,” said Olivia Copelan, MD.

"The ProVee System has the potential to be a first-line interventional therapy for BPH that can be safely and reliably performed in the office setting," says Steven A. Kaplan, MD.

“My goal was very simple. Five years from now, there will be X number of more fathers, brothers, grandfathers who will be having dinners with their families because of what I'm doing, because I will find the cancer early and hopefully make an impact,” says Ashutosh Tewari, MD.