
"The learning curve is fairly quick; you can pick this up pretty easily vs some of the other prostate procedures that can take a little bit more time to learn how to use," says Matthew E. Sterling, MD.

"The learning curve is fairly quick; you can pick this up pretty easily vs some of the other prostate procedures that can take a little bit more time to learn how to use," says Matthew E. Sterling, MD.

"in general, we can use a simpler regimen [of testosterone replacement therapy] and achieve normal levels," says Peter N. Tsambarlis, MD.

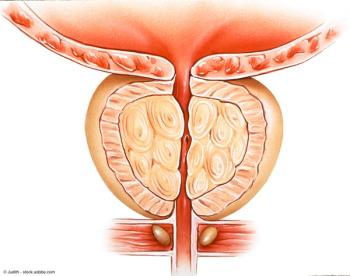
“What we found was that the rate of complications due to infection were 2.6% with the transrectal approach, and 2.7% with the transperineal,” says Badar M. Mian, MD.

"There are situations where you can use a biparametric or noncontrast approach; most of them you will prefer still to use an approach with contrast," says Leonardo Kayat Bittencourt, MD, PhD.

“With 2 years of follow-up, we saw that there was no difference in these 2 groups in terms of overall survival, metastasis-free survival, or recurrence-free survival,” says Saum B. Ghodoussipour, MD.

"Probably the most surprising finding was actually that there were several videos created by health care professionals that contain misinformation," says Alexandra Tabakin, MD.
“We’re in a very exciting time for those of us who take care of patients with bladder cancer. There are a lot of new emerging treatment options,” says Vikram M. Narayan, MD.

“In this study, we sought to compare our early outcomes with transperineal prostate biopsy compared to transrectal,” says Saum B. Ghodoussipour, MD.

"We had interest in trying to look at mechanisms and seeing if the obvious question is, well, if obesity is associated with progressing cancer, can we disrupt that link if we help men lose weight in a healthy way," says Jill Hamilton Reeves, PhD, RD, CSO.

"The limitation of [TURP] is you're shaving out prostate tissue in a layer at a time, and you stop when you think you're deep enough, whereas with an Aquablation, you map all that out ahead of time," says Brian Friel, MD.

“It seems that DRE does not add a clinically or statistically significant [benefit] to PSA testing alone in detecting prostate cancer,” says Shahrokh F. Shariat, MD.

"We have information today from a number of well-powered, well-designed prospective studies showing that performing an MRI before the decision to do the first biopsy adds value," says Leonardo Kayat Bittencourt, MD, PhD.

“Our hope is to really change the practice of medicine,” says Jim C. Hu, MD, MPH.

"Overall, our conclusion is we observed more benefit in apalutamide vs abiraterone," says Mehmet Asim Bilen, MD.

"I think these results particularly apply to practicing urologists that have the opportunity to train residents," says Kathryn Marchetti, MD.

“The patients with CDK12, the combination had a PSA50 of about 83% compared to the ABI/placebo of about only 62%,” says Neal D. Shore, MD.

"We identified that in our site, we were ordering almost 1600 cystoscopy packs. A lot of the materials that were in those packages were unnecessary for an outpatient procedure," says Malissa Williams.

“We wanted to do a modeling analysis using patient-level data to see if we can estimate whether or not there is a long-term cure or overall survival benefit for these patients,” says Daniel M. Geynisman, MD.

“My goal was very simple. Five years from now, there will be X number of more fathers, brothers, grandfathers who will be having dinners with their families because of what I'm doing, because I will find the cancer early and hopefully make an impact,” says Ashutosh Tewari, MD.

"Overall, our conclusion is, in this real-world analyses, more patients treated with apalutamide survive by 24 months following treatment initiation compared to enzalutamide," says Mehmet Asim Bilen, MD.

"In other words, we expected a higher infection rate after transrectal biopsy, however that 1.4% with our current sample size, we weren't powered to detect a significant difference," says Jim C. Hu, MD, MPH.

"I think it's important to try to mix up your visits with patients that you think might be a little shorter, like a vasectomy consult, vs a new patient visit for infertility that may take a little bit longer, so that you don't run over time," says Helen L. Bernie, DO, MPH.

"Male residents do about 100 more cases over the 4 years of urology-specific training than female residents, which is a significant difference," says Kathryn Marchetti, MD.

“We see the pathways of PD-1 resistance being explored across oncology. Kidney cancer is not especially leading the way on that,” says Mayer Fishman, MD, PhD.

“We looked at MRD negative patients, MRD positive patients, and their ultimate clinical response to see if it could be predictive of recurrence-free survival,” says Vikram M. Narayan, MD.

"What we found was that the obedience to the upgrading criteria of PI-RADS as they are today resulted in a better overall outcome for all the patients that were included in the study," says Leonardo Kayat Bittencourt, MD, PhD.

“The American Cancer Society suspects that over 300,000 men will be newly diagnosed with prostate cancer this year, which is still a lot,” says Adam B. Weiner, MD.

"I think people don't understand how exhausting it is for people to manage these symptoms day in and day out," says Leslie Rickey, MD, MPH.

"In this study, we found no difference in patient-reported bowel toxicity in men receiving radiation plus relugolix vs radiation plus leuprolide," says Sagar A. Patel, MD.