
“At its core, [the book is] a love letter to my patients. It's all the things that I didn't have time to tell them in a 15-minute office visit,” says Martha Boone, MD.

“At its core, [the book is] a love letter to my patients. It's all the things that I didn't have time to tell them in a 15-minute office visit,” says Martha Boone, MD.

Experts explore PSMA's significance in prostate cancer imaging, covering its expression, limitations, and transformative role in detecting even low PSA recurrences with PSMA-PET technology.

In this introductory dialogue, Naveen Kella, MD, and Dr. Shadi Esfahani, MD, MPH, discuss PSMA-PET's transformative role alongside conventional techniques in prostate cancer imaging.

"You have to take care of those basic needs, because if not, you're not going to have the space to react differently when you're getting triggered," says Diana Londoño, MD.

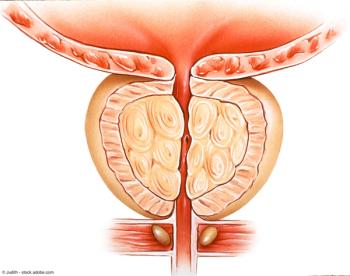
“We're going to be able to treat many more patients who suffer from BPH/LUTS with these less invasive options,” says Dean S. Elterman, MD, MSc, FRCSC.

"Mentorship plays a huge role, and as someone who's interested in academics in the future, I think it's important to remember the influence that you can have on shaping young minds," says Niki Parikh, MD, MBA, MSBA.

“The world of surgery makes a person quite disciplined,” says Martha Boone, MD.

In the third installment of this series, Amar U. Kishan, MD, discusses clinical factors to consider in the use of perirectal spacing for patients receiving hypofractionation or SBRT, and outlines unmet needs.
"I would say the take-home message from this study is that HoLEP uptake has nearly doubled from 2016 to 2019," says Jenny Guo, MD.
“It's a really exciting time for people who are interested in BPH/LUTS,” says Dean S. Elterman, MD, MSc, FRCSC.

Closing out their discussion on how treatment and management of advanced prostate cancer affects their clinical practice, expert urologists consider how the therapeutic landscape continues to evolve and look toward future evolutions in care.

Expert panelists share their perspectives on recent challenges with staffing and turnover in their urology practice and consider how these particular barriers may be overcome, including recruiting and hiring additional advanced practice providers.
"Interestingly enough, we found that PVP accounted for nearly a third of BPH surgeries back in 2016. This number drastically decreased to just 0.7% of all BPH surgeries in 2019," says Jenny Guo, MD.

"Only 25% of our respondents felt that sexual health curriculum provided an adequate fund of knowledge to address any of the sexual health concerns of patients," says Niki Parikh, MD, MBA, MSBA.

"If you've got a difference, pay attention to the size and direction. If you have a massive difference between groups in terms of outcome, but only a small difference in terms of baseline characteristics, that's worth talking about," says Andrew J. Vickers, PhD.

“Our identity is not just about a title; it's not just about that role. We are much bigger than that,” says Diana Londoño, MD.
"We had the idea of doing a scoping review of office-based BPH stents, as this is becoming a new and evolving hot topic in the area of male functional urology," Dean S. Elterman, MD, MSc, FRCSC.

Benjamin H. Lowentritt, MD, FACS, shares background information on micronized abiraterone and discusses its role in the evolving prostate cancer treatment landscape.

"I've always written to just process emotions," says Martha Boone, MD.
“In terms of trying to help patients access the services, the biggest part is just being aware of what's available where you work,” says Sarah P. Psutka, MD, MS.

“I think it's extremely exciting to be part of something that is possibly practice changing, potentially field changing,” says Sandip M. Prasad, MD, MPhil.

“It's really important to pay attention to what's off balance,” says Diana Londoño, MD.

"We're interested in cause; that's why we often are doing observational research. Authors never face that head on, and don't really come to grips with it," says Andrew J. Vickers, PhD.
“I can tell you from a patient standpoint, I think we all agreed across the panel, there's going to be tremendous enthusiasm from patients about a nonsurgical option,” says Sandip M. Prasad, MD, MPhil.

Key opinion leaders briefly review the key challenges in scheduling leuprolide administration for patients with advanced prostate cancer, including treatment delays, disease breakthrough, and insurance reimbursement, and share solutions to overcome these challenges.

Experts outline their clinical approach to identifying treatment failure in patients on initial pharmacologic treatment for OAB and strategies for subsequent treatment selection.

Shared insight on the current state of telehealth and how its use affects treatment selection and followup for patients with advanced prostate cancer.
“Patients just need to be educated that you don't have to live this way,” says J. Welles Henderson, MD, FACOG.
"Given the time constraints and financial constraints of working in the systems that we all work within, trying to make it easier to get patients to these adjuvant services that do exist and making sure we capitalize and utilize those is critical," says Sarah P. Psutka, MD, MS.

“I think it's a very novel finding, and something completely new to urologic oncology, that a nonsurgical ablative option inside the body can actually make tumors go away,” says Sandip M. Prasad, MD, MPhil.