
Treatment with TARA-002 was associated with a 100% high-grade CR at any time in BCG-unresponsive participants.
Benjamin P. Saylor is associate editor of Urology Times, an Advanstar Communications publication.

Treatment with TARA-002 was associated with a 100% high-grade CR at any time in BCG-unresponsive participants.

Clarius Mobile Health said it will be demonstrating the application at the AUA Annual Meeting in Las Vegas, Nevada.
“Oftentimes, [during] the very first visit, we are talking a lot. I am learning what's going on with them," says Anna Myers, CNP.

Take a look through several of the notable phase 3 trials in progress that will be spotlighted at AUA 2025.

The use of onabotulinumtoxinA (onabotA, Botox) for the treatment of overactive bladder comes with several important considerations.

“Like any disease state, you want to make sure you have the right diagnosis; otherwise, you're not going to have a successful treatment plan," says Karyn S. Eilber, MD.

We preview several noteworthy P2 presentations in the urologic oncology space.

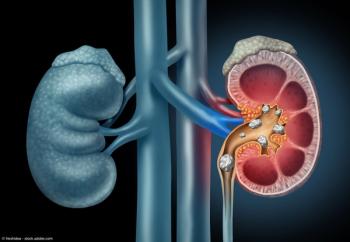
“You absolutely need to have a CT scan prior to the surgery to best identify and really intimately understand the kidney’s anatomy," says Perry Xu, MD.
Merrill discusses the evolving non–muscle invasive bladder cancer treatment space.

"There really wasn't a difference in in surgical outcomes. The patients tolerated it very well,” says Joshua J. Meeks, MD, PhD.

Christian Gratzke, MD, explains why an app shows promise for patients with lower urinary tract symptoms.

“The benefit of being here at the University of Minnesota is that we have a bunch of different types of settings to be able to trial this," says Hailey Frye.

“I feel a lot of providers, with Antiva being available, have unfortunately reserved use of this great FDA-approved agent for BCG-unresponsive patients because of the supply issue with BCG," says Suzanne B. Merrill, MD, FACS.

Betty Wang, MD, provides insight on 3 presentations that she believes “may be game changing” in urology.
"We can improve urinary tract infections considerably with behavioral modification," says Anna Myers, CNP.

“I would say the take-home message for this study is that prescribing tamsulosin for a week prior to an anticipated surgery that involves flexible ureteroscopy is a very simple practice that certainly is within standard of care within pediatric urology," says Kate H. Kraft, MD, MHPE, FACS, FAAP.

“It definitely makes it easier for providers [to counsel patients]," says Landon Trost, MD.

“When I talk to physicians outside of urology, as well as within urology, much of the hesitation with using Cost Plus Drugs is that it seems complicated to use, when in reality, the process is actually very simple," says Raymond Xu, MD.

"A lot of people are using [single-use ureteroscopes] nowadays, and part of it is because it really enhances our ability to provide guaranteed care, because we don't have to rely on the reusability of scopes," says Perry Xu, MD.

A lookahead of the notable FDA decisions and conferences slated for Q2 2025.

"We recognize that an 11% increase in success may not seem that clinically significant, but I think every little bit helps," says Kate H. Kraft, MD, MHPE, FACS, FAAP.

"I'm all for this great effort by ImmunityBio to provide us with an alternative option,” says Suzanne B. Merrill, MD, FACS.

“I think we now have really robust data showing that earlier treatment intensification with combination regimens does lead to improved survival for patients with metastatic hormone-sensitive prostate cancer," says Dr Louise Kostos.
"For other health care professionals aiming to advocate for equitable changes within their system, it's really important to just start conversations about what you're noticing," says Hailey Frye.

"In a practice like mine, where approximately 30% of the practice is low testosterone, it'll have actually very little negative effect," says John P. Mulhall, MD.

“What's really cool about overactive bladder is that, it's not like high blood pressure. They do not have to leave this office with a pill in hand," says Anna Myers, CNP.
“One important aspect to get across…is that access to this EAP is pretty easy," says Suzanne B. Merrill, MD, FACS.

“High risk, non–muscle invasive bladder cancer carries a significant risk of recurrence and progression. This emphasizes the need for careful patient selection, especially when we are considering bladder-sparing approaches," says Neeraja Tillu, MD.

"This now clarifies and substantiates the fact that there are not increased risks from a cardiovascular standpoint with [testosterone] therapy, at least at the doses studied," says Landon Trost, MD.