"A lot of times…decreased desire is affected by everything else: pain with sex, orgasm, arousal. Because if none of that is good, then desire isn't going to be good either," says Anna Myers, CNP.
Benjamin P. Saylor is associate editor of Urology Times, an Advanstar Communications publication.
"A lot of times…decreased desire is affected by everything else: pain with sex, orgasm, arousal. Because if none of that is good, then desire isn't going to be good either," says Anna Myers, CNP.

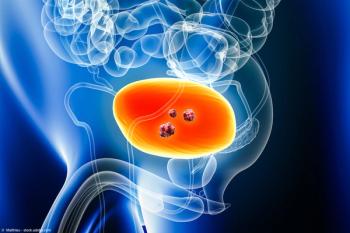
“The impact on bone health is really significant with long-term androgen suppression," says Dr Louise Kostos.

“I think we can really use AI in several different facets of endourology," says Perry Xu, MD.

"I hope that these new guidelines and the removal of the black box warning on testosterone therapy will help more physicians feel comfortable providing testosterone therapy to men," says Helen L. Bernie, DO, MPH.

"When we compared the 2 groups, those that received tamsulosin and those that did not, we did find a significant difference with regard to success rates," says Kate H. Kraft, MD, MHPE, FACS, FAAP. .
“In 5200 men, very clearly, definitively, irrefutably, it has been shown that testosterone therapy is not associated with MACE over the course of the 12 to 24 months after commencement of testosterone therapy," says John P. Mulhall, MD.

"We found that female patients, Black patients, and patients with non-private insurance had a decreased odds of receiving opioids,” says Hailey Frye.

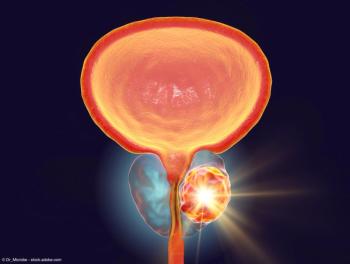
"Personally, I think monitoring and analyzing PSA kinetics is a great one because it's cheap and it's readily available,” says Dr Louise Kostos.

"4 years following radiation therapy, there is a 25% lower hazard of bowel disorders and a 46% lower hazard of related procedures [in patients who received a spacer],” says Michael R. Folkert, MD, PhD.

“Identification of significant predictors [of upstaging] has improved our pre-op counseling," says Neeraja Tillu, MD.

"I think that testosterone is really a medication that can be life changing for so many men, says Helen L. Bernie, DO, MPH.

“The main challenge at the moment is patients are being diagnosed with metastatic disease far earlier than they would have been otherwise, and therefore [are being] considered for combination systemic therapy potentially years earlier than they would have been if we just looked at conventional imaging," says Dr Louise Kostos.

"We need to be aware that patients have options for treatment of high-risk biochemical recurrence, and in order to identify that they have high-risk biochemical recurrence...we need to calculate PSA doubling time,” says Alicia Morgans, MD, MPH.

"I'm so excited about them finally removing this boxed warning," says Helen L. Bernie, DO, MPH.

“For someone that might be looking at getting into sacral neuromodulation, and has had some reluctance in the past, this does simplify the procedure somewhat," says Colin Goudelocke, MD.

"In terms of how I select patients, I really look at the timing of metastatic disease, so whether it's metachronous or synchronous and the volume, and I think at this stage, the data are most robust for the synchronous and high-volume patients," says Dr Louise Kostos.
"I would also like us to be able to reliably use even smaller scopes, but keep them efficient," says Amy E. Krambeck, MD.

"It is important for us to ask patients whether they want to intensify or not, and not make assumptions," says Alicia Morgans, MD, MPH.

"[The lack of] a battery makes it ultra small. That's really important," says Colin Goudelocke, MD.

"It was a really interesting paper to develop and write, because over the past decade, there's been such a paradigm shift in the treatment of prostate cancer," says Dr Louise Kostos.
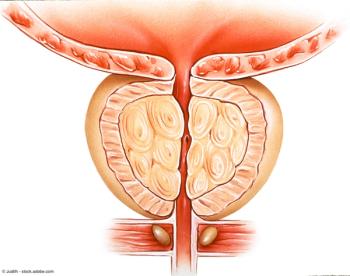
"[Urologists] really need to understand how big the prostate is and how big of a surgery that they're looking at," says Amy E. Krambeck, MD.
Total detection rate was 36% (13/36) in the ultralow PSA group and 51% (47/93) in the low-PSA group.

Robert J. Motzer, MD, reported that median PFS was 16.4 months in the nivolumab plus cabozantinib arm (95% CI, 12.5-19.3) vs 8.3 months in the sunitinib arm (95% CI, 7.0-9.7) (HR=0.58, 95% CI, 0.49-0.70).

Median PFS was 35 months in the MDT plus SOC group vs 21 months in the SOC alone group.

PSMA staging did not appear to have a significant impact on radiation therapy utilization.

“Among active surveillance patients, 82% are metastases-free, and 60% were metastases-free and had an intact, unradiated bladder,” said Pooja Ghatalia, MD.

“Over 80% of patients…had at least 2 lines of therapy, so this is a heavily refractory population,” said Toni K. Choueiri, MD, FASCO.
"The results [indicate] that neoadjuvant DV combined with toripalimab had promising efficacy and acceptable safety in patients with HER2-expressing MIBC,” said Xinan Sheng, MD.

ORR was 70% (95% CI, 55-82) in cohort 1 compared with 31% (95% CI, 19-45) in cohort 2.

The pCR was 37.3% (95% CI, 33.2-41.6) in the durvalumab arm and 27.5% (95% CI, 23.8-31.6) in the comparator arm.