OAB and Incontinence
Latest News
Latest Videos

CME Content
More News

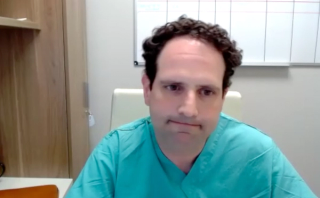
"There are plenty of articles written about stress-induced urgency. I, at the time, only found 1 article written in the gynecologic literature about what they called stand-up urgency," according to Colin Goudelocke, MD.

Colin Goudelocke, MD, offers insight on 2 abstracts from the 2024 Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction Winter Meeting.

"Even the possibility of something really big and revolutionary can still be exciting even if we're in the early stages," says Colin Goudelocke, MD.

Colin Goudelocke, MD, describes an abstract presented at the 2024 Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction Winter Meeting.

“I think 1 size doesn't fit all. We can't make a blanket statement that 1 of those types of therapy is better for all patients than another,” says Suzette E. Sutherland, MD, MS, FPMRS.

Panelists conclude their discussion by reflecting on key learnings and sharing advice for patient-centric management in overactive bladder (OAB) treatment, specifically focusing on effective communication and overlooked aspects of patient care. They offer guidance to other providers on enhancing patient experiences, particularly with procedures like Botox. The episode wraps up with each expert sharing their final thoughts and anticipations for advancements in OAB treatment in 2024, highlighting their commitment to addressing patient needs in this evolving field.

In the intervention group, the HRQOL score changed by 23.9 points between baseline and week 13, from 18.4 to 29.5.

“I think the long and short of it is we know tibial nerve stimulation works, we're just trying to identify what's the best way by which we can deliver it conveniently and cost effectively to the patient,” says Suzette E. Sutherland, MD, MS, FPMRS.

Tepidimonas was notably associated with more severe urinary incontinence episodes, suggesting a potential marker for identifying individuals at risk for more severe symptoms.

In this discussion, Dr. Kennelly, Dr. Kevin Benson, and Dr. Karyn Eilber share their approaches to post-procedure care and follow-up for overactive bladder (OAB) treatments. They detail the patient experience immediately after the procedure, the role of nursing and support staff, and methods for guiding patients through the recovery process, including managing potential complications and effective communication strategies. Additionally, they address challenges in patient adherence to follow-up visits, share insights on assessing treatment effectiveness during these visits, and discuss their strategies for enhancing patient engagement and satisfaction in their practices.

In this episode, Dr. Kennelly, Dr. Kevin Benson, and Dr. Karyn Eilber discuss their strategies for ensuring patient comfort during overactive bladder (OAB) treatment procedures. They delve into the roles of clinical staff, the setup of the procedure room, and how they address patient needs and concerns to create a reassuring environment. The experts also share their experiences in handling challenges during procedures, illustrating how they've adapted their practices based on patient feedback to maintain a patient-centric focus throughout the treatment process.

According to Axonics, commercial sales of the R20 system in Europe are expected to begin in mid-April.

“Currently, in the area of tibial nerve stimulation, there are only 2 FDA approved options,” says Suzette E. Sutherland, MD, MS, FPMRS.

"We're very much looking forward to being able to clinically implement these algorithms, both on the OAB side and the antibiotic resistance side," says Glenn T. Werneburg, MD, PhD.

Panelists discuss the importance of patient-centric approaches in the procedural treatment of overactive bladder (OAB). They share their practices in preparing patients for procedures, including patient education, shared decision-making, and tailoring pre-procedure instructions, with a focus on managing patient expectations and addressing fears. The episode emphasizes the role of the clinical team in ensuring patient comfort, highlighting practical considerations, real-world experiences, and best practices for optimizing patient-centered care in OAB management.

Experts share their long-term clinical experiences with intravesical botulinum toxin type A therapy, particularly emphasizing quality of life, patient satisfaction, simplicity, safety, and the comfort patients find in its non-permanent nature.

The therapy, known as Autologous Muscle Derived Cells for Urinary Sphincter Repair (iltamiocel), involves a medical procedure in which a participant’s own muscle cells are collected, processed, and then injected into the tissues of the urinary passage.

The odds of SUI recurrence following MUS were 17% to 24% among patients with childbirth vs 15% to 22% among patients without childbirth

"We're really enthusiastic on the overactive bladder end and on the antibiotic resistance end, but much more broadly, [AI is] set up to help us counsel our patients better and help us to improve outcomes for our patients as well," says Glenn T. Werneburg, MD, PhD.

Artus is an artificial urinary sphincter for the treatment of patients with moderate to severe urinary incontinence.

In this insightful episode, Dr. Kennelly engages with Dr. Eilber and Dr. Benson in a comprehensive discussion of sacral neuromodulation and transcutaneous and posterior tibial nerve stimulation therapies used in the treatment of OAB, including their mechanisms, patient reception of FDA-approved devices, overall evolution and current practices implementation in clinical settings.

Dr. Kennelly, Dr. Kevin Benson, and Dr. Karyn Eilber share their experiences in the use of intravesical botulinum toxin type A as a treatment option for overactive bladder (OAB) into treatment plans. They provide insight into identifying optimal candidates, the outcomes they have observed, and benefits and risks, including strategies for managing these risks. They explore the decision-making process in guiding patients through various treatment options, considering individual lifestyles and preferences.

"Our outcomes showed 71% of patients achieved dry or near dry results in 6 to 12 weeks," says Nissrine Nakib, MD.
"What we found was that we were able to identify patients who responded vs didn't respond to the treatment with a high degree of accuracy," says Glenn T. Werneburg, MD, PhD.

"I would say that the biggest take-home is that many of our patients are using social media for their health care information, and this may influence their preferences [and] their decision-making," says Alexandra Tabakin, MD.