
"Anecdotally, I would say that many providers actually prefer the functionality of the single-use cystoscopes," says David Barquin, MD.

"Anecdotally, I would say that many providers actually prefer the functionality of the single-use cystoscopes," says David Barquin, MD.

“One of the biggest things that this brings us to for an update of upper tract disease is biopsy alone of an upper tract tumor is not good enough anymore--we must risk stratify these patients,” says Katie S. Murray, DO.
“The way to move the organization forward is to listen to learn, not to win,” says J. Stuart Wolf, Jr., MD, FACS.

"In [bladder cancer], many women's diagnosis is delayed because their hematuria or microscopic hematuria is blamed on urinary tract infections rather than cancer," says Amy Luckenbaugh, MD.

"A unique aspect of AUA guidelines is the robust methodological review," says Todd M. Morgan, MD.

"It's really critical to recruit and retain diverse talent in urology to improve patient care and our health care system overall," says Alexandra Tabakin, MD.
Glenn T. Werneburg, MD, PhD, discusses 2 abstracts from the 2024 SUFU Winter Meeting.

“I think ultimately, when we think about when do we deliver MDRT and to whom, it comes down to a goals of care discussion,” says Angela Jia, MD, PhD.

Raveen Syan, MD, highlights 2 sessions that she took part in during the 2024 AUA Annual Meeting in San Antonio, Texas on urodynamics in the context of the VALUE trial and the new wave of percutaneous tibial nerve stimulation devices.

"We identified 12 discrete workflow steps for outpatient flexible cystoscopy, with 5 of those being able to be eliminated by the transition to the single-use scope," says David Barquin, MD.

"Our first question is, in patients who were on the GLP1R agonists for a prolonged period of time, were those patients at increased or decreased risk of developing the most common GU malignancies?" says Laura Bukavina, MD, MPH.

"I would say the take-home message is that usage of this mobile health platform could potentially improve patient quality of life and compliance with recommendations," says Jenny Guo, MD.

“Cancer is a journey which is very emotional as much as it is physical. And not only for the patients, but it is also for their caregivers, whoever that person is,” say Joy Maulik, CRNP.

"The other was that we found that about half of the patients in the CIS cohort and two-thirds of those in the Ta/T1 or papillary cohort had bladder preservation, meaning they were able to avoid cystectomy," says Vikram M. Narayan, MD.

"What we saw among over 400 patients [was] that indeed, subcutaneous heparin did not increase the hematoma chance, but it reduced the chance to have venous thrombotic events," says Thairo Pereira, MD.

"I think these findings suggest that for clinicians who treat a lot of older adults with neuromodulation, caution should be exhibited when recommending the single-stage approach," says Leo Dreyfuss, MD.

“Certainly, there are more and more radioligands coming out not only in prostate cancer, but in other cancers related to urology, and I think that's going to be the next big wave,” says Timothy A. Richardson, MD.

“When we looked at the risk of bleeding and takeback for fulguration, the reported rate was 0.46%. Less than 1% of patients had any significant bleeding,” says Dean S. Elterman, MD, MSc, FRCSC.

"We saw that Black men within this cohort had lower Decipher scores across all ages and Gleason scores different than what had been reported in other data sets, which was interesting," says Samuel L. Washington III, MD, MAS.
“But more importantly, there are patients who have no insurance, there are patients who have no other resources and are maybe even on the poverty line. We feel, importantly, that we have an obligation that the drug be made free for these patients in the United States,” says Patrick Soon-Shiong, MD.

"We found that the GetWell patients have shown increases in their Wisconsin Stone Quality of Life scores, or the WISQOL score, of about 3 points from baseline to 6 months," says Jenny Guo, MD.

"In the study, about two thirds of the residents did undergo PNE and one third underwent Stage 1, and those who underwent PNE were less likely to progress to device implant than Stage 1," says Leo Dreyfuss, MD.

"In our commercial all-comers cohort of patients undergoing Aquablation, efficacy was similar to and safety was improved compared to the WATER I and WATER II clinical trials," says Shawn H. Marhamati, MD, MS.

"One of the main summaries/focuses of this discussion was, how do we create action to improve screening, and what that actually means," says Samuel L. Washington III, MD, MAS.

"[The care plan] incorporates patient-specific data to reinforce dietary management, fluid intake, and medication adherence based on the patient's 24-hour urine collection results," says Jenny Guo, MD.

"So I think these findings overall are reassuring and support the use of neuromodulation in this population," says Leo Dreyfuss, MD.
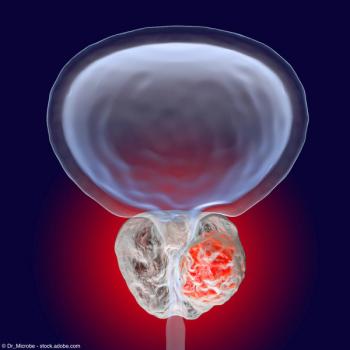
"So, there's a lot of evidence to point to the androgen receptor being an important player in at least developing this disease," says Edward M. Messing, MD.

“Along those lines, we've taken away the traditional step therapy that has dictated overactive bladder care for quite some time,” says Ariana L. Smith, MD, FPMRS.

“The 2018 AUA guidelines for testosterone therapy that were co-chaired by Dr. John P. Mulhall say that we have an absence or a paucity of data on using testosterone therapy on active surveillance,” says Helen L. Bernie, DO, MPH.

"The biggest take home point is that patients with node-positive disease at the time of radical prostatectomy are a heterogeneous group of patients," says Daniel A. Triner, MD, PhD.