Articles by Urology Times staff
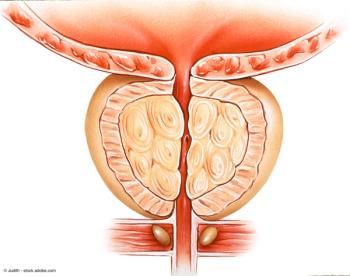
"I think the main takeaway from this study is that prostate cancer is not as rare in trans women as we think it is, and that we really need to be giving this population the time that they deserve, and that they should be screened equally to their cis male counterparts," says Matthew Loria.


"At Northwestern Medicine, we have very extensive and very deep experience with PET-PSMA-based imaging," says Edward M. Schaeffer, MD, PhD.

Dr. Heidenberg discusses the recent Urology paper, “The Impact of Standard vs Early Apical Release HoLEP Technique on Postoperative Incontinence and Quality of Life.”

"We concluded based on our 36-month evaluation that nadofaragene was an option for patients who had BCG-unresponsive disease," says Colin P.N. Dinney, MD.

“The main takeaway is that we want to be working with [transgender and gender-diverse patients] the same way that we are working with cisgender folks,” says Matthew Loria.

"In the moment, I think it's important to take a deep breath and try not to just be reactive," says Anne M. Suskind, MD, MS, FACS, FPMRS.

“The actions taken by those matched over 80% of the time. It seemed like what they saw, knowing the history, was a reasonable approximation of what an in-person urologist would do,” says Tracey L. Krupski, MD.

"We've been doing a lot of work at Johns Hopkins using high-dose testosterone therapies to treat patients with metastatic prostate cancer," says Mark C. Markowski, MD, PhD.

"We ultimately found that trans women from between the ages of 50 and 65 who were on hormone therapy had a 2.5-fold decreased risk of prostate cancer compared with cis men," says Matthew Loria.

“I think in actuality it's going to have to be one of our trained APPs going to these sites on a scheduled day, like the third Wednesday of every month,” says Tracey L. Krupski, MD.

"Like any test, it's really a very powerful tool. It's just how you deploy the tool," says Edward M. Schaeffer, MD, PhD.
“The hope is that we can collaborate with folks who might be interested in trying nadofaragene plus something else, something that compliments the mechanism of action, so that we can build upon what we have now,” says Vikram M. Narayan, MD.

"We hope that this paper encourages urologists to rethink non definitive treatment/active surveillance for prostate cancer and consider definitive treatment options earlier in the treatment pathway based on evidence that has accumulated," says Mital Patel, MD.

“I think 1 size doesn't fit all. We can't make a blanket statement that 1 of those types of therapy is better for all patients than another,” says Suzette E. Sutherland, MD, MS, FPMRS.

"We know that surgical intervention for ureteroscopy for both renal and ureteral stones does result in a relatively rapid and also quite substantial improvement in quality of life that does exceed preoperative baseline," says Justin B. Ziemba, MD, MSEd.
"We really aimed to affect 3 different contraindications and instead achieved retirement of the entire policy, which, we think, really opens up this wonderful technology to literally hundreds of thousands more patients across the country," says Arpeet Shah, MD.

“I would just say that urologists should be focusing much more on the total amount of pattern 4, if they have that information available, than on the ratio of pattern 3 and 4, and therefore the grade group,” says Andrew J. Vickers, PhD.

"Because it takes advantage of a viral vector and is delivered as a gene therapy product, what it can do is it can have sustained release of IFNα2b in the bladder," says Vikram M. Narayan, MD.

"The point is healthy, adaptive changes that are sustainable, that you can keep off, because we don't want that rebound/regain," says Jill M. Hamilton-Reeves, PhD, RD, CSO.

"PSMA PET imaging is used in the initial diagnostic staging and then in subsequent cases where there can be a recurrence after primary treatment.," says Edward M. Schaeffer, MD, PhD.

“The 1 tweak that's different for our model is that the trained urologist is watching the cysto at the same time as the nurse practitioner is doing it,” says Tracey L. Krupski, MD.

"As most of us know, 1 in 8 couples undergo issues pertaining to fertility, and in about half of those cases, there is a male factor involved, resulting in infertility," says Akash Kapadia, MD.

"We must do more to help surgeons prepare for the impact of adverse events before they happen," says Kevin Turner MA DM FRCS(Urol).

"One notable finding was that veterans may not have access to the same quality of prostate cancer care as the US general population," says Olubiyi Aworunse, MD, MPH, PhD.

“I think the long and short of it is we know tibial nerve stimulation works, we're just trying to identify what's the best way by which we can deliver it conveniently and cost effectively to the patient,” says Suzette E. Sutherland, MD, MS, FPMRS.
"I continue to be regularly surprised at just how much surgeons are affected when things go wrong, and how little surgeons engage with existing support mechanisms," says Kevin Turner MA DM FRCS(Urol).

"What we did find was that a preoperative ureteral stent, and when we did semi rigid ureteroscopy initially, seemed to be protective against worse symptoms," says Justin B. Ziemba, MD, MSEd.

"Every time I leave the meeting, I just feel reinvigorated, refreshed, and excited about this field that we're a part of," says Raveen Syan, MD, FPMRS.

"The implications for urology, and every specialty, are immense. It does improve care, and it helps the patient. I think this is what it will be, it just may take some time," says Vipul Patel, MD.