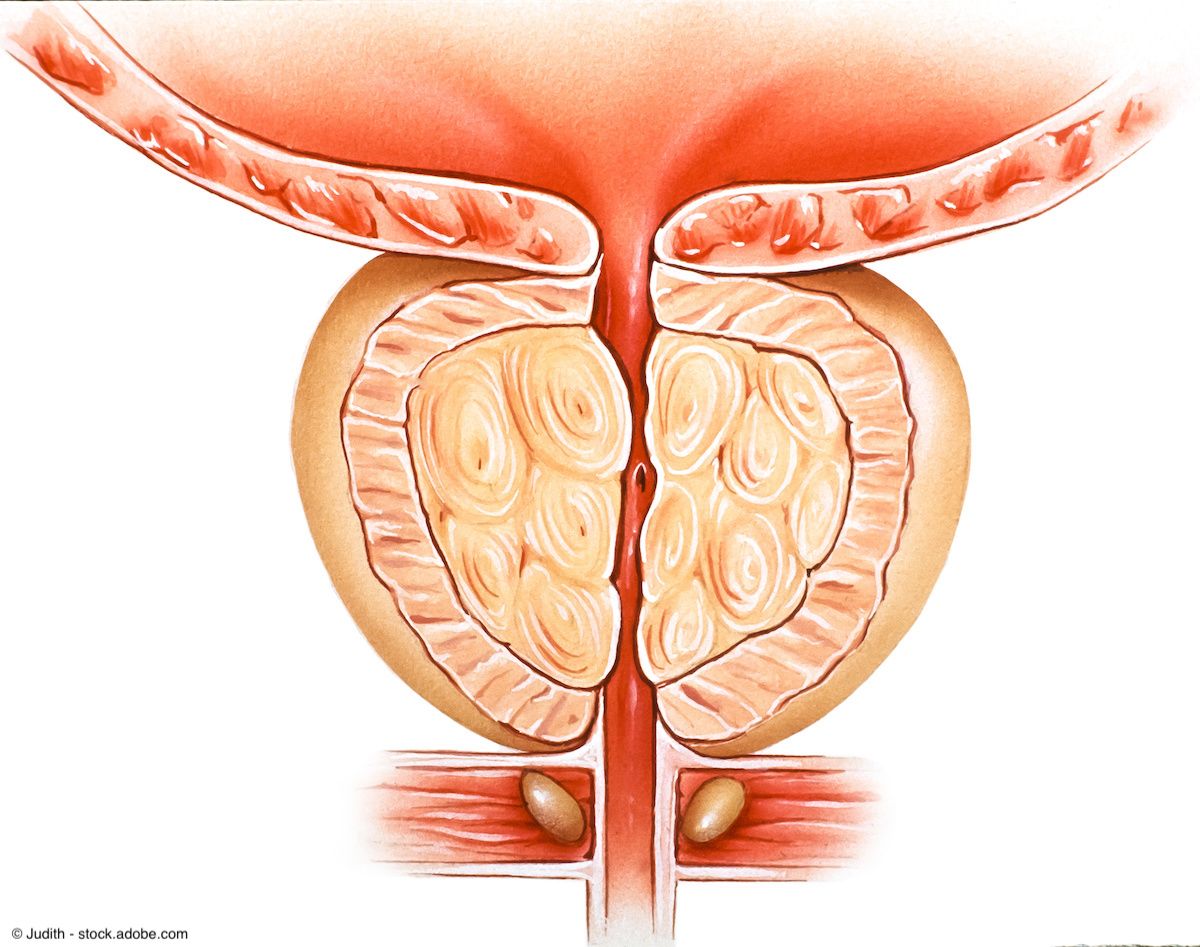
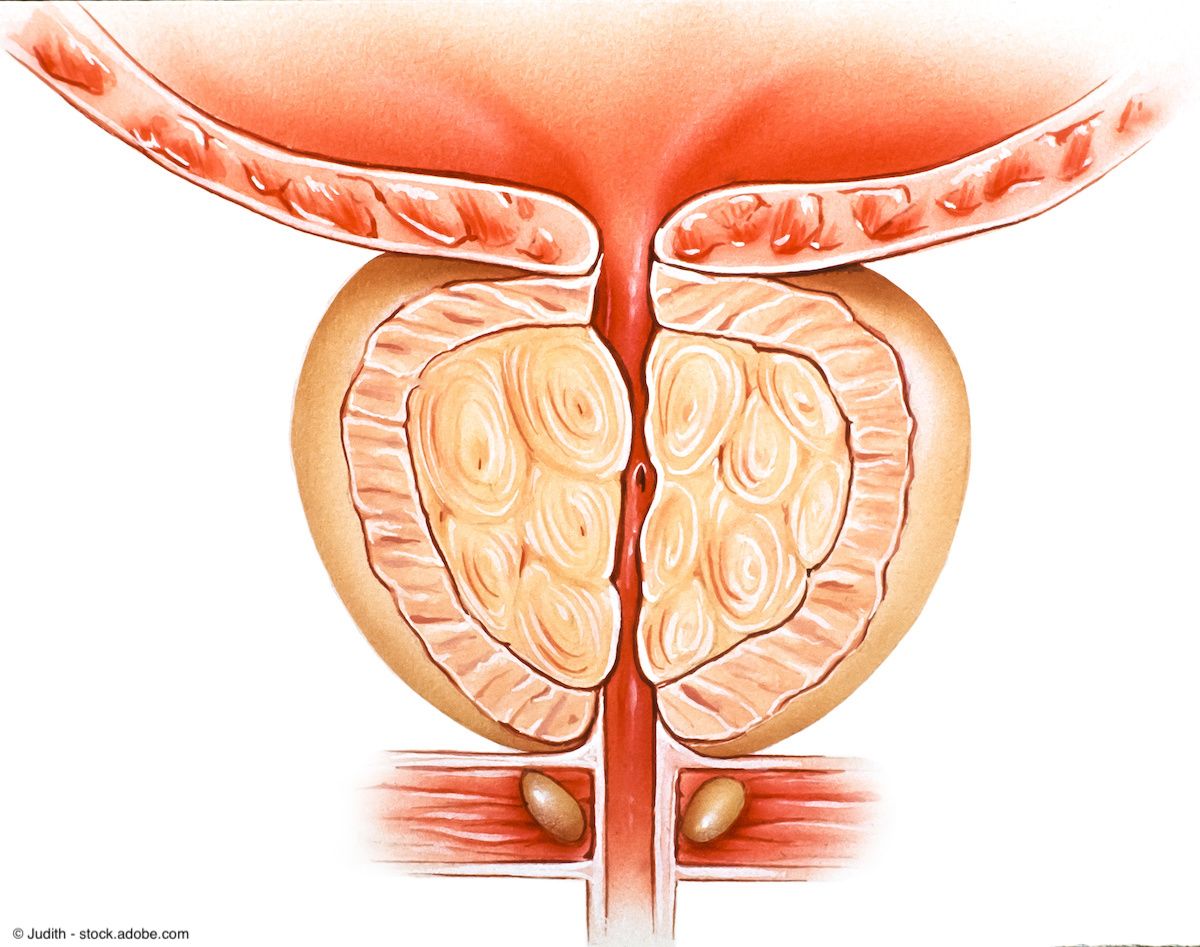
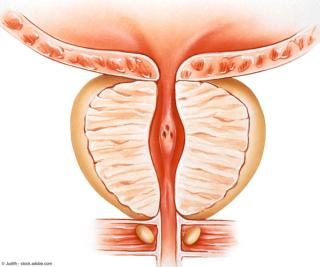
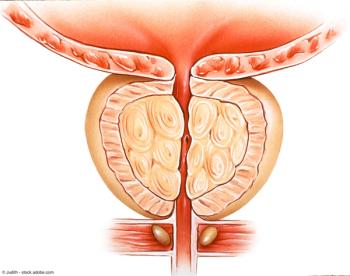
Benign Prostatic Hyperplasia
Latest News
Latest Videos

CME Content
More News
“Overall, I'd say these shorter-term outcomes at 6 months look to be very similar to those outcomes measured with the smaller glands. In a sense, at least within this range, volume may not be a deal breaker,” says Kevin T. McVary, MD.

As the year comes to a close, we revisit some of this year’s top content on benign prostatic hyperplasia in urology.

“There's a bit of an unmet need about the impact of Rezum in these bigger prostates,” says Kevin T. McVary, MD.

All patients had prostates greater than 80 mL and had not responded to prior medication therapy.

The center will offer a comprehensive range of treatments, including prostate artery embolization for men suffering from benign prostatic hyperplasia with very large prostates.

“It's 2023. We have a lot of other options. I'm not really sure that would be my frontline therapy for my dad or a family member,” says Kevin C. Zorn, MD, FRCSC, FACS.

Support for the NICE recommendation included 5-year results from the WATER trial, which showed that Aquablation had strong efficacy and safety vs transurethral resection of the prostate in patients with BPH.

The inclusion of iTind is reflected in a newly added statement on temporary implanted prostatic devices.

Both the LUTS/BPH and testicular cancer guidelines were updated based on the availability of new literature, as identified through an AUA Update Literature Review process.

"The findings suggest that we may need to view urinary symptoms differently, possibly with an emphasis on earlier treatment,” says Blayne Welk, MD, FRCSC, MSc.

Questions spanned urologic conditions such as benign prostatic hyperplasia, overactive bladder, erectile dysfunction, kidney stones, Peyronie disease, and recurrent urinary tract infections.
“Aquablation is safe and effective based on several years of research,” said urologist Zein K. Nakhoda, MD.

In this installment, Kevin Zorn, MD, FRCSC, FACS, highlights his disease-specific practice, BPH Canada, which he designates as a “one-stop shop” for patients with benign prostatic hyperplasia.

“We're going to be able to treat many more patients who suffer from BPH/LUTS with these less invasive options,” says Dean S. Elterman, MD, MSc, FRCSC.

Aquablation is a “minimally invasive procedure [that] is safe with long-term durability and a low-side effect profile,” said urologist Dennis Bentley, MD.
"I would say the take-home message from this study is that HoLEP uptake has nearly doubled from 2016 to 2019," says Jenny Guo, MD.
“It's a really exciting time for people who are interested in BPH/LUTS,” says Dean S. Elterman, MD, MSc, FRCSC.
"Interestingly enough, we found that PVP accounted for nearly a third of BPH surgeries back in 2016. This number drastically decreased to just 0.7% of all BPH surgeries in 2019," says Jenny Guo, MD.
"We had the idea of doing a scoping review of office-based BPH stents, as this is becoming a new and evolving hot topic in the area of male functional urology," Dean S. Elterman, MD, MSc, FRCSC.

"The next-generation Optilume BPH Catheter System offers a safe and effective new, minimally invasive treatment for BPH, reducing urinary obstruction with a low rate of sexual or other adverse effects," says Steven A. Kaplan, MD.

"[These findings] will encourage us to continue to offer bladder neck incision to these patients if their bladder neck appears narrow after laser enucleation," says Nicholas S. Dean, MD.

"Of the patients who underwent a prophylactic bladder neck incision... none of those patients developed a bladder neck contracture at 14 months of median follow-up," says Nicholas S. Dean, MD.

Data among patients with follow-up of greater than 48 months demonstrated an IPSS reduction of 45.2% from baseline to 79 months following treatment.

The minimally invasive surgical therapy Optilume was recently approved by the FDA for the treatment of lower urinary tract symptoms secondary to BPH.

Data showed a decrease in patient symptoms following Aquablation procedures, with an average IPSS of 22.6 at baseline compared with 6.8 at 5-year follow-up.