“When a patient knows that there are so many tools that are there for people, it gives them hope. It gives their caregivers hope,” says Joy Maulik, CRNP.
“When a patient knows that there are so many tools that are there for people, it gives them hope. It gives their caregivers hope,” says Joy Maulik, CRNP.

"It's a little tedious to find these patients, but it's really critical. Otherwise, you're not going to get reimbursed for these therapies," says Jason Hafron, MD.

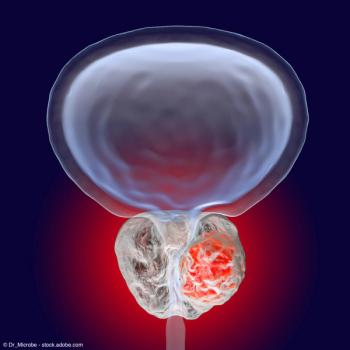
"Bladder cancer is exploding. [It] is exciting, it's changing, and we're just at the start of this," says Jason M. Hafron, MD, CMO.

“We then talked a little bit about BCG unresponsive disease, which is a really hot topic,” says Gautam Jayram, MD.
"When we look at focal therapy in general, the better we're able to see, localize, identify and risk stratify prostate cancers, the better we're able to treat them and offer more personalized and focal treatments," says Arvin George, MD.

“We're really excited as robotic surgeons, because this will be the first time in a couple decades that there'll be competition for robots, and that's only going to make things better,” says Ronney Abaza, MD, FACS.

In this episode of Speaking of Urology, former MLB player Dave Winfield shares lessons he’s learned throughout his professional baseball career and his work in philanthropy.

"We...talked a little bit about BCG-unresponsive disease, which is a really hot topic; a lot of trials and a lot of data are coming there," says Gautam Jayram, MD.

“The guidelines have changed. They used to be called third-line therapies, and they're no longer quote "third-line" anymore, based on the new guidelines that have come out,” says Kari Bailey, MD.
“You have to be balanced in what to embrace vs what not. It is easy to be wowed by new things," said Scott Eggener, MD.

“Part of the reason that we created this Working Group Session is to essentially highlight the role that APPs can play in building men's health practices,” says Andrew Y. Sun, MD.
“I would say, about 10 years ago, there was a real skepticism, a healthy skepticism, I would say, in the beginning. Now that has slowly changed into optimism,” says Arvin K. George, MD.

“I think that it is upon us as urologists to try to start to embrace this clinical accomplishment, and that being trying to make our patients as stone free as possible,” says Tom Mueller, MD.

“It's exhausting and it's overwhelming, but traction has been gained and continues to be gained and we are making some meaningful, tangible differences,” says Mara R. Holton, MD.

"The Inflation Reduction Act has changed the landscape, and we really still don't understand what those implications are going to be," says Mara R. Holton, MD.

“We have definitely seen significant trends toward transparency in hospital pricing, and in regulations designed to promote that, as well as PBM reform,” says Mara R. Holton, MD.

“This year in particular, we really attempted to highlight a novel conversation about financial toxicity,” says Mara R. Holton, MD.

"This is the 15th year [of LUGPA,] and I think I've gone maybe 12, 13 years in a row or so, almost every year," says Lawrence Gervasi, MD.

"The providers–the nurses and the physicians and the extenders–are checking out and burning out, which is affecting quality and delivery. To me, it's a national health care crisis," says Scott A. MacDiarmid, MD, FRCPSC.

"We are really engaged on ensuring that a lot of the progress that had been made and the care that was delivered through the pandemic is able to continue on," says Joshua Langston, MD.

"Being able to utilize advanced practice providers to extend us, to take care of our patients, [and] to treat them in a way that is beneficial and satisfying for them as a job is really important," says Neal Patel, MD.

“One important takeaway that we wanted to hammer home is that AI will not replace urologists, but urologists who use AI will replace those that don't,” says Neal Patel, MD.

"This is our biggest meeting ever in our 15-year history [with] almost 1100 people here," says Evan R. Goldfischer, MD, MBA, FACS.

"This all started because of the tidal wave of new therapies that are coming out for bladder cancer," says Jonathan Henderson, MD.

"There was also an emphasis on using pathways and navigation to help facilitate this large group of patients that are being seen by urologists," says Arpeet Shah, MD.

"They found that about 68% of the patients with a PSA less than 1 actually had a positive test. And that's really important," says Jason M. Hafron, MD.

"Patients shouldn’t be making the decision to do active surveillance without understanding what that means and what their other options are,” one panelist said.

“Radiation therapy continues to expand its role, especially if you start talking about [patients with] the ultra high–risk [prostate cancer] or node-positive [disease] and beyond,” says Daniel Spratt, MD.

“We went to medical school to take care of patients, not to service the computer, which is what we do for a large part of our daily work," said Inderbir Gill, MD.

"I think it may provide better care. What has been shown though, with some things, is that it can make mistakes and tries to cover them up, and that can be a problem also," says E. David Crawford, MD.