
"Over a third of Americans actually use some kind of what we term complementary or alternative medicine approach," says Raevti Bole, MD.

"Over a third of Americans actually use some kind of what we term complementary or alternative medicine approach," says Raevti Bole, MD.
“There are a lot of other ways to look at bel-sar with other immunotherapy agents, other combinations, to truly help prevent patients needing to go to the operating room,” says Gary D. Steinberg, MD.
"The 5-year data from STOMP showed that about a third of men could go 5 years without requiring ADT, which is exciting," says Bridget F. Koontz, MD, FASTRO.

Oliver Sartor, MD, discusses how 68gallium PSMA-11 PET is indeed the preferred imaging modality for confirming eligibility for lutetium therapy, but when unavailable, alternative options such as F-18 PSMA PET, conventional bone scintigraphy, or CT/MRI may be considered, albeit with potential limitations in sensitivity and specificity.

“We really need to do a better job of destigmatizing these conversations so guys are comfortable asking their providers [about sensitive health issues],” says Justin Dubin, MD.

“Now for muscle-invasive [disease], how I counsel patients on surgery when they're a man vs a woman is almost completely different, because their anatomy is very different,” says Ava Saidian, MD.


"We found actually that patients who underpredict their curve during the initial visit, prior to having a formal measurement of their penile curvature, actually ended up having a higher satisfaction following treatment," says Jake Miller, MD.
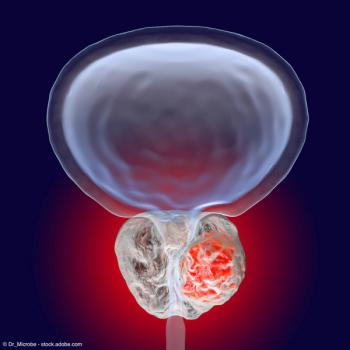
Panelists discuss how the increased use of androgen receptor–targeted therapy in clinical practice may impact the effectiveness of PARP inhibitor combinations like talazoparib in the TALAPRO-2 study, while also addressing safety concerns, potential differences in trial populations, and the need for future studies to optimize treatment approaches for various metastatic prostate cancer patient subgroups.
Panelists discuss how the PROfound trial (NCT02987543) demonstrated the efficacy and safety of olaparib monotherapy in metastatic prostate cancer patients with homologous recombination repair gene alterations, highlighting its potential as a targeted treatment option and its impact on the landscape of precision medicine in prostate cancer management.

Michael Jenson, PA-C, gives an overview of the Surgical Impotence Management Strategy program at Minnesota Urology.

"We were actually interested in looking at what was the impact of prostate cancer on sexual quality of life for female partners of patients," says Stacy Loeb, MD, MSc, PhD (hon).

"I think it requires the adequate staff, and then also the development of a practice pattern for how chaperones are used," says Ellen Cahill, MD.

Dhingra discusses the utility of PSMA-PET imaging when treating patients with prostate cancer.
Panelists discuss how metastatic castration-sensitive prostate cancer (mCSPC) is defined by its sensitivity to androgen deprivation therapy, while metastatic hormone-sensitive prostate cancer (mHSPC) emphasizes the cancer’s responsiveness to hormone treatment, highlighting the nuanced differences in patient management strategies.

"Most of us are focusing on our healthspan and our lifespan, but we also need to think about our sexspan," says Mohit Khera, MD, MBA, MPH.

"We wanted to study if Dupuytren's contracture has any effect at all in Xiaflex treatment," says Muhammed A. Moukhtar Hammad, MBBCh.

"We had 66 respondents, and 48% of those did say that they had functionally limiting pelvic pain...for 14 days out of a given month at least," says Sarah Ponce.

"I think it's really important when we're prescribing any medication to our patients to really have a good idea of what they can expect," says Evan Panken, MD.
“The other thing that we believe will be important to see is it not only effective where we inject a tumor and turn the light on in the tumor, but will there be abscopal effects throughout the bladder?” says Gary D. Steinberg, MD.

Hehemann gave a talk titled “Burnout/Impostor Syndrome” at the 2024 SMSNA Fall Scientific Meeting in Scottsdale, Arizona.

"There are no formal guidelines on whether chaperone use is recommended or is mandatory," says Ellen Cahill, MD.

“I think one of the biggest challenges women have in general in terms of diagnosis of bladder cancer is that it tends to be delayed,” says Ava Saidian, MD.

The panelist discusses how the limited availability of 68gallium PSMA-11 gozetotide in clinical practice poses challenges and suggests potential strategies to increase accessibility, such as expanding production facilities, improving distribution networks, and exploring alternative radiotracers with longer half-lives.
“Over 80% of the patients are greater than 50% improved, and 50% [had] over [a] 75% reduction in UUI episodes,” says Cindy L. Amundsen, MD.

"If you are going to be an inclusive leader...it's important that you think about those gaps in education and hopefully try to fill those," says Denise Asafu-Adjei, MD, MPH.

Panelists discuss how PARP inhibitor monotherapy trials like TALAPRO-1 (talazoparib) and TRITON-3 (rucaparib) have demonstrated efficacy and safety in treating metastatic prostate cancer patients with homologous recombination repair gene alterations, providing important insights into targeted therapy options for this specific patient population.
Panelists discuss the characteristics of an ideal multidisciplinary team for managing BCG-naive, high-risk non–muscle-invasive bladder cancer (NMIBC), emphasizing the need for oncologists and urologists to collaboratively prepare for successful patient outcomes across different markets, while also identifying necessary educational resources and highlighting adverse events that require attention in preparation for product launches.
Panelists discuss existing and upcoming data in non–muscle-invasive (NMIBC) bladder cancer treatment, including insights from the BladderGATE trial on frontline use of PD-1 inhibitors combined with BCG and the enfortamab vedotin plus pembrolizumab combination while also addressing the significance of clinical complete response as an end point and the potential role of circulating tumor DNA in future evaluations.