
“The notable finding was that the combination was well tolerated,” says Kelly L. Stratton, MD.

“The notable finding was that the combination was well tolerated,” says Kelly L. Stratton, MD.

“This technology is truly a transformational opportunity for urology,” says Melissa R. Kaufman, MD, PhD, FACS.

“I think Aquablation is safe. It’s efficacious, especially in these large prostates,” says Kevin Zorn, MD, FRCSC, FACS.

“For some men, it's very important to make sure that they have an antegrade ejaculation and this is a treatment modality that we're able to offer them,” says Andrew Higgins, MD.
“What's novel about the iTind system is [that] it's one of the first treatments that [can] be deployed through a flexible cystoscope, as well as the fact that there is no permanent energy or permanent foreign body that's left within the prosthetic urethra,” says Bilal Chughtai, MD.

“This device is unique in that because it's done during real-time MRI imaging while the patient is in the MRI machine, [we] can monitor the temperatures achieved by our treatment in real time and make adjustments in real time. What that means is that we're able to determine areas that will be sensitive to the treatment, both cancer and areas from a quality-of-life perspective,” says Behfar Ehdaie, MD.
“We need to treat our patients with stones, both medically and surgically,” says Glenn M. Preminger, MD.

“This is the beginning of an exploration and an identification,” says Steven A. Kaplan, MD.

Interim results from the ROBUST III trial were presented at the 2021 AUA Annual Meeting.

“We are truly embarking at this moment on the next frontier in urology with these types of cellular therapies,” says Melissa R. Kaufman, MD, PhD.

“We recommend doing the spot cautery,” says Andrew Higgins, MD.
“Even in patients that have only been single-stone formers, especially those that have required surgical stone removal, we believe that medical prevention is warranted to prevent recurrent stones,” says Glenn M. Preminger, MD.

“You have tradeoffs with every device that you use,” says Amy E. Krambeck, MD.

“Tramadol is a mixed-class medication and it has weak opioid agonist activity. Normally, we consider that a safer option compared to other opioids, but it's actually a pro drug, so it has to be metabolized to have an effect,” says Sarah F. Faris, MD.
Michael S. Cookson, MD, previews the 2021 AUA Annual Meeting, with a focus on prostate, bladder, and kidney cancer. His in-depth analysis covers the plenary sessions, late-breaking abstracts, and other abstracts of interest.

“It was nice to use the military health system to look at the population, which tends to be very diverse…[It allowed] us to get pretty large numbers to make some better conclusions about what’s already been established in this population,” says David A. Klein, MD, MPH.
Get ready for the 2021 AUA annual meeting with this preview of non-malignant topics.

“We have to be really careful prescribing tramadol and be aware that [it] can have really variable effects for patients,” says Sarah F. Faris, MD.
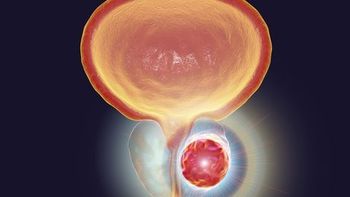
“When a man initially presents with metastatic disease, or fails initial systemic therapy, our approach has to be different. We are more concerned that their disease is more aggressive,” says Leonard Gomella, MD.

“Through these 2 small punctures, we can manipulate the device with the methodology to sample the entire prostate, both anterior apical and the posterior regions, where we find the vast majority of our cancers,” says Matthew A. Allaway, MD.

“Appropriately selecting your patient will result in a successful telehealth visit,” says Nitya E. Abraham, MD.

“A lot of clinicians are seeing transgender and gender-diverse people in their practice, whether it’s urology, whether it’s primary care, whether it’s other subspecialties…[They should have an understanding] that transgender and gender-diverse people are at a higher risk of a multitude of mental health diagnoses,” says David A. Klein, MD, MPH.

“The transperineal [prostate biopsy] approach is safer because the needles are passed through the perineal skin…so, we can sterilize that skin and if we enter through that passageway, we mitigate, if not eliminate, the risk of infection and sepsis,” says Matthew J. Allaway, MD.

“Transgender and gender-diverse people are at a higher risk of a multitude of mental health diagnoses, [which] really lends itself to a sensitive psycho-social history regardless of the specialty,” says David A. Klein, MD, MPH.

“The 3 major barriers we face [are] training, equipment, and reimbursement,” says Matthew A. Allaway, MD.

“The notable feature was that the bleeding risk is very small. In our particular group, it was less than 1%,” says Jai Seth, MD.

In this interview, Nicole L. Miller, MD, discusses her institution’s enhanced recovery after surgery protocol for ureteroscopy, which eliminates the use of opioids in patients undergoing this common procedure.

“This is an important form of providing health care, especially for people who have a lot of limitations in coming for in-person visits,” says Nitya E. Abraham, MD.

“From a clinician’s perspective…these medications and these diagnoses happen when there’s not enough care from the start,” says David A. Klein, MD, MPH.
“We found a majority of patients with televisits were satisfied, with many saying it was easy to schedule, easy to comfortably share sensitive information with their doctor, and with the most surprising [finding] being 80% saying they would choose it again over an in-person visit,” says Christina Shin, BA.