Articles by Urology Times staff

“The concept behind the NAXIVA trial was to treat these patients with pre-surgical neoadjuvant targeted therapy with a means of downstaging that venous tumor thrombus, reducing the extent of it to try and make the surgery less morbid to the patient and to potentially improve survival,” says Grant Stewart, MD.

“It is a vaccine that is self-administered by the patient sublingual over 3 months, and that is why it appears to be so safe,” says J. Curtis Nickel, MD.

“This study really demonstrates, for one of the first times certainly in the largest cohort of men ever [studied], that Rezum water vapor thermal therapy is a viable option to treat men with very large prostates bigger than 80 mL,” says Dean Elterman, MD, MSc, FRCSC.
“I think these results are very encouraging [in] that we may be able to bridge the gap in prostate cancer treatment, in which we're selective [and] prostate gland-sparing,” says Behfar Ehdaie, MD, MPH.

“The take-home message is vibegron is a very safe drug and there are no concerns about any kind of cardiovascular adverse effects,” says Michael A. Weber, MD.

“In general, urologists are really happy people. They love their work, but they're not exempt from the challenges that come with any workplace, especially when you have a lot of different roles, you have a fast environment, and the stakes are high,” says Loren Jean Smith.

“I want to reiterate that this study doesn't necessarily say that 1 approach is better than the other, but it definitely does reinforce some advantages of robotic surgery that have been shown not just in this study, but in other studies as well,” says Peter Chang, MD, PhD.

“[We gave the ES kits out] with the idea that instead of having these people…travel…hundreds of miles to a main hospital for their endoscopy, the urologist could travel to a village with just the smartphone and the endoscope set-up and proceed to do a ton of endoscopy there,” says Ralph V. Clayman, MD.

“The majority of treatments out there don't allow the maintenance of ejaculation after surgery, whereas here, we're at 90% for the small glands…[and at] 81% [for] the men who had prostates above 80 grams,” says Naeem Bhojani, MD, FRCSC.

"This work isn't for one; it is certainly for all,” says Efe C. Ghanney Simons, MD.

“Rather than asking the staff to have a stiff upper lip and cope, we instead tried to focus on uncovering systemic processes that were ripe for change,” says Loren Jean Smith.

“The quality of life overall between the 2 approaches was very similar,” says Peter Chang, MD, PhD.

Ernest Sussman, MD, FACS, explains why all urologists must also be risk managers.
“The data is out to about 2 to 3 years now, so…[it’s] a little bit on the immature side, but it's very promising,” says Bilal Chughtai, MD.

“I think the key [is to not] get rid of financial incentives. I don't think that's possible. [Rather, we should] align financial incentives [so] that [we] can promote what is best for patients,” says Lillian Y. Lai, MD.

“This type of collaboration [between SEER and GPS assay] is a really nice illustration of the types of projects that we should be undertaking in the future,” says Scarlett Gomez, MD, PhD.

“[Rezum] does give men another option, and so I think that's…really what we're focusing on here: giving the option to avoid general anesthesia and to avoid a bigger surgery,” says Michael A. Palese, MD.

“The goal of this research endeavor was to really set forth the background information that would guide the creation of targeted interventions,” says Efe C. Ghanney Simons, MD.

“As health care professionals, we've got…an incredibly important role and responsibility with regards to increasing awareness and education, and then really trying to address the barriers and bring down the barriers,” says Jai Seth, MD.

The noninvasive Oncuria immunoassay predicts response to BCG therapy in patients with intermediate-to–high-risk, early-stage bladder.

Welcome to the first installment of Uranimals, a video series featuring urologists and their pets brought to you by Urology Times. From a dog model to a whole farm of animals, the inaugural episode has an amazing lineup.

“We're getting close, and we hope to have things concluding here soon and then to be able to offer some of these technologies on a on a wider scale,” says Mathew D. Sorensen, MD, MS, FACS.

“This is a successfully completed phase 3 trial in regenerative medicine in our field, and there's demonstrated safety and efficacy for women who have failed previous surgery, a very difficult group of patients for all of us,” says Michael B. Chancellor, MD.

In this video, Laurence Klotz, MD, FRCSC, discusses the miR Sentinel PCC4 Test and how it could change the future of prostate cancer testing.

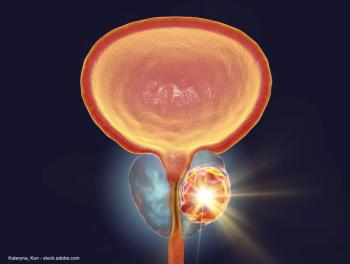
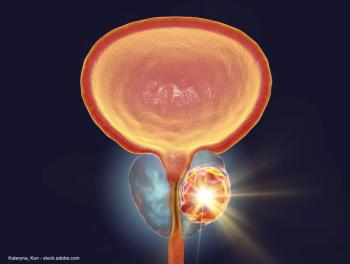
In this interview, Ardeshir (Art) Rastinehad, DO, discusses the current state of focal therapy in prostate cancer, the role of fusion biopsy in pushing the treatment forward, and what institutions looking to implement focal therapy should know.

“It works on the bladder [and] it relieves the symptoms of people who have overactive bladder, but it doesn't do any adverse things to blood pressure or heart rate.” says Michael A. Weber, MD.

“I’m looking forward to comparisons of minimally invasive surgery versus medical therapy, that is, at this point, untapped. It's something which we think we have insight into, but we really don't have good data,” says Kevin T. McVary, MD.

“Our study strongly suggests that telemedicine can become the mainstay of treatment within FPMRS even after the COVID-19 pandemic has ended,” says Christina Shin, BA.

“The activity that we saw with the combination was very promising and…it justifies additional clinical trials to determine whether or not this could have a place in terms of our standard treatment options for patients,” says Michael Schweizer, MD.

“Our data shows that in newly diagnosed men with prostate cancer, yoga improved quality of life [as well as] some immune markers, and [lowered] inflammation,” says Dharam Kaushik, MD.