UTv Videos
“Waiting for others to fix health care is not a good strategy. Instead, be determined to begin your journey to your mountaintop of joy and fulfillment,” says Scott A. MacDiarmid, MD, FRCPSC.

"Even just the process of getting that β3 agonist is going to cost them time and energy and effort that can be quite frustrating and take a lot out of you," says A. Lenore Ackerman, MD, PhD.
“We were actually quite pleased with how well our model performed, particularly in the independent cohort that was separate from our training cohort,” says Eric Li, MD.

"We are optimistic about this study, because it has the potential not just only for vesicovaginal fistula treatment, but it can be also used in the treatment of burns for other fistula types," says Ilaha Isali, MD.
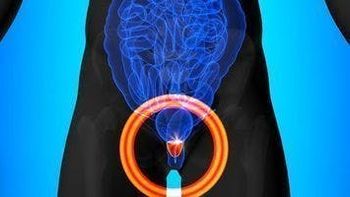
Chandler Park, MD, discusses lessons from the ARASENS and TITAN trials on the use of triplet vs doublet therapy in patients with metastatic hormone-sensitive prostate cancer.

“The first thing I'd say is that we know these devices are safe,” says Colin Goudelocke, MD.

“I think clinicians can really take away that we have more work to be done in this space of evaluating patients with microhematuria, specifically when it comes to looking at assessments of upper tract urothelial carcinoma or renal cell carcinoma,” says Jacob Taylor, MD, MPH.

“We want to minimize our negative biopsies and diagnosis of grade group 1 cancers,” says Rashid Siddiqui, MD.

“I would say that these conditions are highly heterogeneous, and we've identified a number of factors that relate to different ways that the disease progresses and different ways that patients feel about the progression of their disease,” says Alisa J. Stephens-Shields, PhD.

“We might find that there's a certain type of patient that really thrives on interacting with the device and playing an active role in his or her therapy,” says Colin Goudelocke, MD.
“What we need now are biomarkers to know if the medication is going to work or not,” says Park.

"Understanding work productivity and activity impairment in the context of the treatment decisions are vital, not just for the provider who has to counsel on treatment benefits and risks, but also to the patient who's making the ultimate decision," says Angela Smith, MD, MS.

“Collagenase [clostridium histolyticum (Xiaflex)] is a really important part of our treatment armamentarium,” says Matthew J. Ziegelmann, MD.

"From a urology provider perspective, we should be discussing this with our patients [with bladder cancer] as they make their treatment decisions," says Angela Smith, MD, MS.

“I think it's important as urologists to try to understand how we fit into this scheme and how we can participate in value-based care in a meaningful way without negatively affecting patients,” says Avinash Maganty, MD.
Alexandra Sokolova, MD, discusses unanswered questions and next steps with PARP inhibitors in the prostate cancer treatment paradigm.

Arya Mariam Roy, MBBS, discusses the effect of neoadjuvant chemotherapy on overall survival in patients with sarcomatoid bladder cancer.

The phase 2 CaboPoint trial is exploring cabozantinib in patients with locally advanced or metastatic renal cell carcinoma who progressed after first-line checkpoint inhibitor–based combination therapy.

“[Collagenase clostridium histolyticum (Xiaflex)] is an incredibly important part of the treatment armamentarium for Peyronie's disease in the US,” says Matthew J. Ziegelmann, MD.

"The [SWIU meeting] is a meeting that provides updates to all of our members about the exciting initiatives that the organization has been able to accomplish in the preceding year, as well as the initiatives that are planned for the subsequent year," says Akanksha Mehta, MD, MS.

“We do see that the device appears to be clinically efficacious,” says Colin Goudelocke, MD.

"I think there's going to be a rapid adoption of artificial intelligence platforms in our field," says David Sheyn, MD.

“We would like to use all of what we've learned in the MAPP to move back into the space of clinical trials and trying to identify effective therapies for this condition,” says Alisa J. Stephen-Shields, PhD.

“The readers of our paper should really understand that in microhematuria specifically, a lot of the recommendations are based on small amounts of data,” says Jacob Taylor, MD, MPH.

"Where it's feasible and where the patients are eligible, I and others are trying to use alternative therapies, which have probably a similar impact in terms of improving longevity of life for patients [with prostate cancer]," says Praful Ravi, MD, BChir, MRCP.

"The first main finding was after adjusting for individual physician characteristics as well as the characteristics of the actual patient case mix for each physician, we found that small practices performed poorly compared with larger practices," says Avinash Maganty, MD.

“This is a lifetime disease; you want to make sure that the battery not just has long enough life but still has the capacity,” says Colin Goudelocke, MD.

“First, we found that we should not be using voided samples for bladder cancer research,” says Laura Bukavina, MD, MPH.

"We unfortunately did not find any difference in pain scores [after ureteroscopy] at day 1, 2, or 3. We also didn't find any difference in use of rescue medication and rescue narcotic medication," says Karen L. Stern, MD.
