Articles by Urology Times staff

"Looking at the effect of the darolutamide on docetaxel, we didn't see much of a difference in dose reduction, dose modification, or dose hold for docetaxel, telling you that darolutamide didn't really affect the dosing of docetaxel," says Arash Rezazadah Kalebasty, MD.

"We're trying to understand where these new therapeutic agents might fit into our paradigms of care," says John L. Gore, MD, MS.

"This trial did not require a biomarker for entry in, so patients were treated with combination therapy or standard care, which would have been the abiraterone alone, to see if there was a benefit," says Michael S. Cookson, MD, MMHC.

“The effect size for adjuvant nivolumab versus placebo across primary, secondary, and exploratory endpoints is all remarkably stable,” says Matthew D. Galsky, MD.

"The median survival of the combination arm was 16.1 months versus 13.4 months in the standard chemo arm," says Enrique Grande, MD.

“There are a number of trials that we're interested in to develop potentially combining chemotherapy and neoadjuvant immunotherapy,” says Joshua J. Meeks, MD, PhD.

"The MMAI model had significantly improved accuracy and prognostication to discriminate which patients would develop distant metastasis or die from prostate cancer," says Daniel E. Spratt, MD.

“I would ask the practicing urologist to keep an open mind and not be dogmatic about how they've practiced in the past, and to consider the multiple lines of both indirect and direct evidence that exist,” says Surena F. Matin, MD.

"We found that if the patient has normal IsoPSA, he has only 1% of risk of developing clinically significant prostate cancer in a median follow-up time of 18 months," says Nour Abdallah, MD.

“Same-day discharge after partial nephrectomy in properly selected patients is safe and cost effective for both patients and the health system,” says Andrew Wood, MD.

“HIFU also has gone up in its APC, so there's a higher reimbursement for the facility fees for hospital or ASC setting,” says Jonathan Rubenstein, MD.

"The reason that we really focus on prostate cancer is because it's amenable to early screening. Early detection is key in cure," says Janet Kukreja, MD, MPH, FACS.

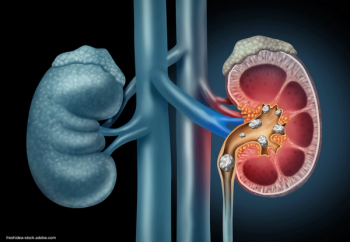
“Based off the questionnaire, [there was] statistically significant worsening quality of life, increased pain, and [increased] pain medicine requirement with a stent compared to without a stent,” says Christopher Allam, MD.

"This scope allowed me to maintain the intrarenal pressures lower than I would originally have done," says Naeem Bhojani, MD, FRCSC.

“I am seeing this process rapidly expand, particularly with the use of the single-port robot, which offers additional benefits to things like pain control and helps to further expedite early discharge,” Andrew Wood, MD.

“There are a couple of nomograms that are good for predicting either T2 or higher disease at time of surgery, so on final pathology, or T3 or higher,” says Suzanne Lange, MD.
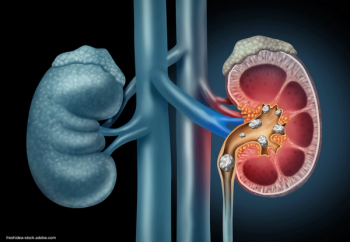
"The biggest take-home message for any urologist who's treating kidney stones is to understand that what we consider to be success may not be what our patients consider to be success," says John Michael DiBianco, MD.

"Before you even start your contract negotiation, I think it's really important to have a negotiation with yourself and understand what's important to you," says Siobhan M. Hartigan, MD.

“I would just burn it into everyone's brain that pain with intercourse is also going to be associated with genitourinary syndrome of menopause,” says Rachel Pope, MD, MPH.

"It may be something that practicing urologists could already start speaking to their patients about," says Siobhan Sutcliffe, PhD, ScM, MHS.

"It wasn't just about the salary number, but what other things are within the contract that could make a huge difference on your practice and your life," says Siobhan M. Hartigan, MD.

“We highlighted that there is building evidence suggesting clinical benefits for lymph node dissection, such as a clear benefit of staging, which allows us to perform better prognostication for patients,” says Suzanne Lange, MD.

"This has the opportunity to really revolutionize the way we treat kidney stone disease via ureteroscopy," says Naeem Bhojani, MD.

"Major bladder reconstructive surgeries have the most room for improvement, particularly surgeries involving a bowel anastomosis; also our major oncologic surgeries—Wilm's tumor resections, those types of surgeries," says Sarah Hecht, MD.

“First and foremost is that same-day discharge appears to be safe. There were no failure-to-rescue events within 24 to 48 hours after discharge outside of the hospital,” says Andrew Wood, MD.

"You have to manage and maintain the other parts of yourself that are not answering all those needs from work," says Jennifer M. Taylor, MD, MPH.

"What really surprised us was that 25% of our Botox cohort had previously undergone nerve stimulation, and those patients were less likely to stop Botox," says Katherine L. Woodburn, MD.

“There's a huge potential role for urologists out there for female sexual health,” says Rachel Pope, MD, MPH.

"We used data from this study to see whether having a greater number of flares independently impacted patients’ quality of life as well as their healthcare seeking activity," said Siobhan Sutcliffe, PhD, ScM, MHS.

The patient was treated as part of a clinical study of the novel MONARCH platform at UCI Health in California.