
“There's a lot of talk about Roe v. Wade affecting the reproductive health of women. This implies that it's also affecting reproductive health decisions for men,” says Sarah Vij, MD.

“There's a lot of talk about Roe v. Wade affecting the reproductive health of women. This implies that it's also affecting reproductive health decisions for men,” says Sarah Vij, MD.

Urinary tract infections (UTIs) are among the most common human infections. But the urine culture, the cornerstone for laboratory diagnosis of UTI, is imperfect.

In an episode of Cleveland Clinic’s Cancer Advances podcast, Christopher Weight, MD, center director of Urologic Oncology at Cleveland Clinic, discusses robot-assisted retroperitoneal lymph node dissection.

"The model that we developed was able to behave as accurately as clinical models that were previously validated," says Nour Abdallah, MD.

“The need for lifesaving organs continues to grow. We continue to increase patients’ options regarding the type of donors. We want them to get this life-changing procedure as soon as possible,” said Alvin Wee, MD.
Cleveland Clinic highlights its use of irreversible electroporation, also known as Nanoknife, in select patients with prostate cancer.

"We found that if the patient has normal IsoPSA, he has only 1% of risk of developing clinically significant prostate cancer in a median follow-up time of 18 months," says Nour Abdallah, MD.

“Same-day discharge after partial nephrectomy in properly selected patients is safe and cost effective for both patients and the health system,” says Andrew Wood, MD.

“I am seeing this process rapidly expand, particularly with the use of the single-port robot, which offers additional benefits to things like pain control and helps to further expedite early discharge,” Andrew Wood, MD.

“First and foremost is that same-day discharge appears to be safe. There were no failure-to-rescue events within 24 to 48 hours after discharge outside of the hospital,” says Andrew Wood, MD.

"Over the past 10 to 15 years, tremendous efforts have gone into robotic surgical innovation to improve perioperative morbidity for patients with bladder cancer undergoing RC," write Andrew M. Wood, MD, and Nima Almassi, MD.

“If outcomes are improved for patients who take this combination — or in patients whose cancer is still progressing after being treated with hormone-based chemotherapy alone — this could be a big step forward in caring for these patients," says Moshe Ornstein, MD, MA.

“As other factors such as access to care, socioeconomic conditions, patient preference, and other unknown confounders might have played a role in the observed disparity, it is still unclear whether overestimating the postoperative eGFR of Black patients contributes to the lower use of nephron-sparing approaches in this population,” the authors write.

Innovation is at the cornerstone for care in Cleveland Clinic’s Department of Urology, and it’s enabling experts to deliver more personalized approaches to patients.

Machine learning isn’t new to medicine or to urology, but its potential remains largely untapped, according to the authors of two new Cleveland Clinic–led studies.

Patients can now undergo prostate surgery with epidural anesthesia and light sedation, known as twilight sleep, without the need for a ventilator general anesthesia.

A team of Cleveland Clinic urologists and pediatric oncologists has developed a streamlined testicular tissue collection and storage process. They have enrolled and cryopreserved testicular tissue for nearly a dozen young patients so far.
“It’s pretty clear that over the past 50 years we've seen innovations in BPH treatment both from the utilization of technology and also from the patient outcome and experience standpoint,” says Bradley Gill, MD, MS.

Shilpa Gupta, MD, explains that the toxicities of sacituzumab govitecan and enfortumab vedotin “are not overlapping.”

In this interview, Howard Goldman, MD, discusses the development of sacral neuromodulation as a treatment for overactive bladder (OAB).

"[Sacral neuromodulation has] changed the treatment of OAB remarkably," says Howard B. Goldman, MD, FACS.

"With the average cost of treatment ranging from $2600 to $3900 per cycle, clinics offering radial wave therapy have an obvious financial incentive to continue marketing despite the lack of evidence of its effectiveness," write Navid Leelani, DO, and Scott D. Lundy, MD, PhD.

Cleveland Clinic specialist discusses the implications of the first published guideline for neurogenic lower urinary tract dysfunction

ADT and other mainstays of therapy for men with castration-resistant prostate cancer may be effective in the management of Skene’s gland malignancy, a rare paraurethral adenocarcinoma.
Kidney transplant surgeon Alvin Wee, MD, MBA, presented findings at the 2022 AUA Annual Meeting
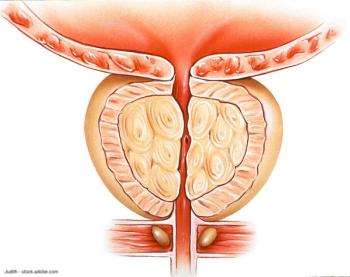
Minimally invasive BPH procedures relieve symptoms and can be done in outpatient settings.

On this episode of Cleveland Clinic’s Cancer Advances podcast, Byron Lee, MD, PhD, discusses optimizing surgical options for patients with bladder cancer.

A 54-year-old transgender woman presented at Cleveland Clinic with vaginal stenosis. She was seeking surgical revision after complications from gender affirmation surgeries performed at other care centers failed to establish a functional neovagina.

Cleveland clinic physicians Rahul Tendulkar, MD, and Steve Huang, MD, provide expert insight on PSMA-PET imaging and explain how it has changed clinical management of patients with prostate cancer.

In this installment, Howard B. Goldman, MD, FACS, discusses the development of multichannel urodynamics testing.