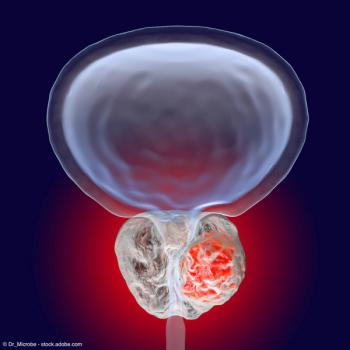
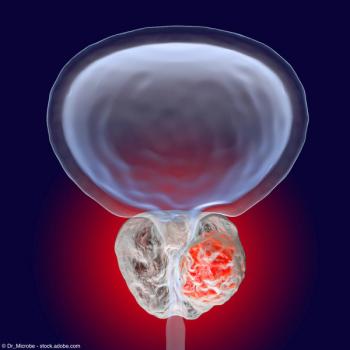
Prostate Cancer
Latest News
Latest Videos

CME Content
More News

New CEASAR findings at ASTRO 2024 show how 3 treatment modalities differ in prostate cancer patient functioning—as well as how patients perceive the issues.


Ga-68 PSMA-11 radiotracer may be a feasible option for SCINTIX radiation therapy in patients whose prostate cancer has spread to the bones.

Follow-up phase 3 analyses support a hypofractionated radiation therapy regimen to conventional dosing in patients with prostate cancer.

The panel concludes by addressing unmet needs in prostate cancer management, with a particular focus on improving risk stratification methods.

"As we expected, the MRIs with contrast were far more expensive," says Benjamin Pockros, MD, MBA.

"The landscape of prostate cancer management has evolved significantly over the past 30 years, with [active surveillance], advances in imaging and genetics, and improvements in the treatment of high-risk disease marking key areas of progress," writes Michael S. Cookson, MD, MMHC.

“Patients in the darolutamide arm did not reach first [radiological progression-free survival] median, but at 24 months, 70[.3]% had not progressed vs 52[.1]% in the placebo/ADT arm,” said Fred Saad, CQ, MD, FRCS, FCAHS.
“Our findings give patients and doctors valuable insights into what to expect after ADT treatment, helping them make informed decisions about managing side effects and improving long-term outcomes," says Amar U. Kishan, MD.

"Of those that met the primary end point, they remained free of progression at a median of 31 months and counting," says Nicholas G. Nickols, MD, PhD.

No patients in the transperineal cohort experienced an infection, compared with 1.6% of patients in the transrectal cohort.

Panelists discuss how the treatment landscape for metastatic castration-resistant prostate cancer (mCRPC) is rapidly evolving through advancements in precision medicine and novel therapies, while emphasizing the importance of ongoing education for community oncologists to stay updated on these changes.

The panel explores promising biomarker research that has the potential to significantly impact patient care in prostate cancer.

Prostate cancer specialists share their insights on anticipated future advancements that could significantly influence prostate cancer management strategies.

"But for physicians considering chemotherapy for which there is equipoise, the Decipher test could be used to swing the decision one way or the other," says Gerhardt Attard, MD, PhD, FRCP.
Patients with at least 1 NE-positive marker were shown to have a worsened rPFS and OS.

“We already have very effective ARPIs available around the world, and this will add to those therapeutic options to try to tailor patients based on their needs [and] their particular profiles,” says Fred Saad, MD, FRCS.
According to the authors, data from the CONTACT-02 trial show that cabozantinib plus atezolizumab may benefit selected patients with mCRPC.

New data from ESMO 2024 support an initial dose of Radium223 prior to chemotherapy among patients with mCRPC.

New findings from the open-label SPLASH trial show patients with mCRPC achieved improved progression-free survival as well as response rates and antigen-specific reductions.
“Today, we're presenting the results of this analysis, and we show that patients who have a high Decipher score derive significant benefit from docetaxel,” says Gerhardt Attard, MD, PhD, FRCP.

Panelists discuss how to address the challenges in providing optimal care for mCRPC patients and how barriers may vary between different healthcare settings, such as rural vs. urban and private vs. public.

Panelists discuss how the dosing and administration of different abiraterone formulations vary, how food-related effects impact treatment efficacy, and strategies to manage these effects for optimal patient outcomes.

The key opinion leaders explore strategies for integrating newly available diagnostic tests into the existing treatment paradigm and patient journey.

The panel examines the significance of biomarkers in assessing therapy outcomes for prostate cancer patients, while also exploring the concept of absolute benefit in metastasis risk when adding androgen deprivation therapy (ADT) to radiation therapy for newly diagnosed cases.