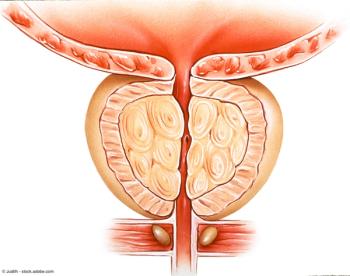
Panelists discuss how regulatory approval of the radium-223 and enzalutamide combination would likely lead to significant guideline updates, particularly in treatment sequencing recommendations for patients with metastatic castration-resistant prostate cancer (mCRPC) with bone-predominant disease and adequate bone marrow function.