
“Part of the reason that we created this Working Group Session is to essentially highlight the role that APPs can play in building men's health practices,” says Andrew Y. Sun, MD.

“Part of the reason that we created this Working Group Session is to essentially highlight the role that APPs can play in building men's health practices,” says Andrew Y. Sun, MD.
“I would say, about 10 years ago, there was a real skepticism, a healthy skepticism, I would say, in the beginning. Now that has slowly changed into optimism,” says Arvin K. George, MD.

“I think that it is upon us as urologists to try to start to embrace this clinical accomplishment, and that being trying to make our patients as stone free as possible,” says Tom Mueller, MD.

"We only have so much time with our patients, but we want to show them that we support them," says Ava Saidian, MD.
"I cannot wait to see what the SMSNA is going to have in store next year," says Helen L. Bernie, DO, MPH.

“Certainly, I think when you have these inherent challenges or biases in the reimbursement aspects, it has to beg the question, does this or how will this impact the future of acquisition or passing down of these newer technologies?” says Kevin C. Zorn, MD, FRCSC, FACS.

"We found that almost half of them had suspicious findings as defined by the radiologist, but also that the positivity rate for PSAs below 0.5 were around 35%," says Eric Li, MD.
"I would basically look at these 3 things as the major things to be coming up," says Jitesh Dhingra, MD, FRCEM.

“On a lesion level, there were still more lesions detected with PSMA-PET, but not on a patient level,” says Jeremie Calais, MD, PhD.

"We were trying to understand how veterans were making decisions about germline testing for their prostate cancer," says Daniel Kwon, MD.

“I think this is the future, and if we don't go down that path and we don't explore, we're not going to make it better for us and for the patients,” says Geoffrey N. Sklar, MD, FACS.

"We were really surprised that we found that the anxiety components in the depression questions in those 3 questionnaires really improved drastically when we compared them to pretreatment vs post treatment," says Andrew C. Peterson, MD, MPH.

"For urologists that are interested in implementing Aquablation into their armamentarium, I am very envious, because anyone who is going to start doing Aquablation now is going to be using the HYDROS System," says Ravi Munver, MD.

"This is quite reassuring to show that there's no statistically significant influence of BMI in actual complications," says Muhammed A. Moukhtar Hammad, MBBCh.

“For us, being able to know where the cancer is allows us to target it, and I think that lets us be much more effective with our treatment,” says Bridget F. Koontz, MD, FASTRO.

"I think it would be really nice if we did have standardized guidelines on who could serve as a chaperone," says Ellen Cahill, MD.

"Patients, in general, have been extremely happy, and the one thing that I think keeps them happy is I'm continually evolving with how I give the information," says Michael Jenson, PA-C.

“There's not an increase of reimbursement across all provinces in Canada that met up or was at par with the cost-of-living index,” says Kevin C. Zorn, MD, FRCSC, FACS.

"Over a third of Americans actually use some kind of what we term complementary or alternative medicine approach," says Raevti Bole, MD.
“There are a lot of other ways to look at bel-sar with other immunotherapy agents, other combinations, to truly help prevent patients needing to go to the operating room,” says Gary D. Steinberg, MD.
"The 5-year data from STOMP showed that about a third of men could go 5 years without requiring ADT, which is exciting," says Bridget F. Koontz, MD, FASTRO.

“We really need to do a better job of destigmatizing these conversations so guys are comfortable asking their providers [about sensitive health issues],” says Justin Dubin, MD.

“Now for muscle-invasive [disease], how I counsel patients on surgery when they're a man vs a woman is almost completely different, because their anatomy is very different,” says Ava Saidian, MD.


"We found actually that patients who underpredict their curve during the initial visit, prior to having a formal measurement of their penile curvature, actually ended up having a higher satisfaction following treatment," says Jake Miller, MD.

Michael Jenson, PA-C, gives an overview of the Surgical Impotence Management Strategy program at Minnesota Urology.

"We were actually interested in looking at what was the impact of prostate cancer on sexual quality of life for female partners of patients," says Stacy Loeb, MD, MSc, PhD (hon).

"I think it requires the adequate staff, and then also the development of a practice pattern for how chaperones are used," says Ellen Cahill, MD.

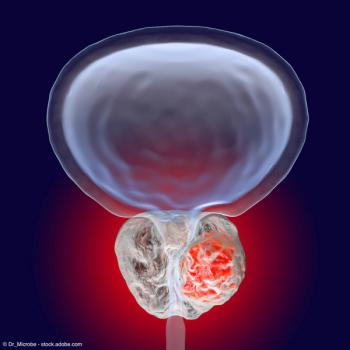
Dhingra discusses the utility of PSMA-PET imaging when treating patients with prostate cancer.

"Most of us are focusing on our healthspan and our lifespan, but we also need to think about our sexspan," says Mohit Khera, MD, MBA, MPH.