
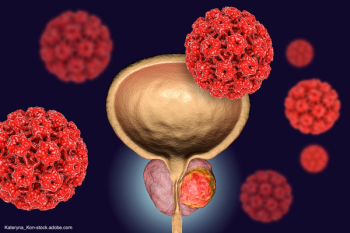
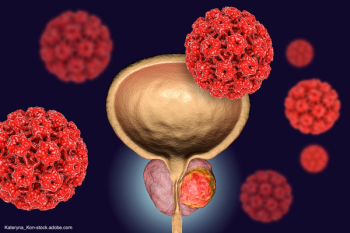
“So many patients with prostate cancer qualify for genetic testing, but it's currently underutilized,” says Stacy Loeb, MD, MSc.

“So many patients with prostate cancer qualify for genetic testing, but it's currently underutilized,” says Stacy Loeb, MD, MSc.

"The other things that are important are to use the privilege that you have as a senior mentor, even as a mid-level or junior mentor, to help open doors for people and make connections," says Mark S. Litwin, MD, MPH.

“This study is one of the most highly anticipated of all of the metastatic hormone-sensitive setting trials that we have going on at this time,” says Alicia Morgans, MD, MPH.

“The benefits can be reaped by the vast majority of patients and because we're really undertreating these patients, we need to make a conscious effort to overcome whatever barriers are facing us,” says Alicia Morgans, MD, MPH.

"The first takeaway I would say is that there is not only a lot of passion for each of these different areas in our society, but also there's a lot of expertise and experience within our urologic community from which we can all draw upon," says Manoj Monga, MD, FACS.

“These are codes that had not been updated in decades—since they were originally written,” says Jonathan Rubenstein, MD.

“I think really identifying who's going to benefit from what combination for how long is going to be important,” says Stephanie Berg, DO.

Dr. Freedland closes his discussion by highlighting remaining unmet needs in mCRPC treatment and providing some clinical pearls for community oncologists treating patients with the disease.

Dr Stephen J. Freedland muses on how the utilization of AR pathway inhibitors and docetaxel in earlier lines of prostate cancer treatment has impacted subsequent treatment selection in mCRPC.

Stephen J. Freedland, MD, explains the treatment regimen he would have chosen for the patient with mCRPC in the presented case and outlines which factors, including clinical data, inform his treatment decision-making.

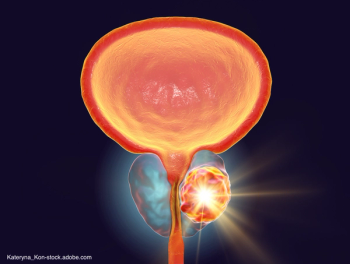
Dr Stephen J. Freedland reviews the available treatment options for patients with metastatic castration-resistant prostate cancer (mCRPC), visceral disease, and no actionable genomic alterations, who received prior treatment with docetaxel and AR-targeted therapy.

Stephen J. Freedland, MD, presents the case of a 67-year-old man with metastatic prostate cancer and give his initial impression.

Several treatments are being explored across these trials, including pembrolizumab, nivolumab, enfortumab vedotin, durvalumab, avelumab, and cabozantinib.

“Now, we only have 1 code set that we have to worry about instead of 2 code sets,” says Jonathan Rubenstein, MD.

“We don’t want to subject patients to a therapeutic strategy that they are unlikely to benefit from,” says Atish D. Choudhury, MD, PhD.

“Practices need to be aware that they need to be able to budget for those who perform in-office services that have very little clinical labor, but may have a high practice expense overall,” Jonathan Rubenstein, MD, says.
“Every year, we see our reimbursements go down. Every year, there seem to be some sort of patch,” says Jonathan Rubenstein, MD.
“There are a slew of ongoing trials looking at 177Lu-PSMA-617 in earlier stages of disease,” says Praful Ravi, MB, BChir, MRCP.
“We have to remember that this is not a cure for prostate cancer…right now, it is another tool in the toolbox,” says Praful Ravi, MB, BChir, MRCP.

“We found many factors in urology that were associated with the inability to follow through with a video visit,” says Kevin Shee, MD, PhD.
Slovin says what’s interesting about the CAR-T platform she’s been exploring is that “we see pretty exquisite sensitivity to the cancer cells.”

"[Low-grade prostate cancer] is a really interesting field right now," says Kevin Shee, MD, PhD.
“The takeaway from that talk was that it's critically important to review drug plan options, particularly if the patient's on a high-cost drug,” says Kelly L. Stratton, MD, FACS.

“The idea of generally screening everyone right now is not only costly, but it's not recognizing the fact that this comes with a lot of limitations,” says Mark A. Moyad, MD, MPH.

Ashley E. Ross, MD, PhD, provides an overview of his institution’s new protocol for this subset of patients.

“[The 2022 Huggins Medal Lecture from Harry Herr, MD] was a fascinating talk, and something that I think anyone could learn from,” says Kelly L. Stratton, MD, FACS.

“It was vitamin E and selenium in 2011-2012. There was a lot of hype about it. People were very excited. They lost their excitement in urology about it, but then along came vitamin D,�” says Mark A. Moyad, MD, MPH.

“I think [it was a] great opportunity to catch up on what is going on with PSMA-PET and theranostics and then also understand that that landscape will change over the near future,” says Kelly L. Stratton, MD, FACS.

“It really was a multidisciplinary effort to pull the data together [and] provide the clinical implications [of] the genetic markers,” says Veda N. Giri, MD.

“It's very interesting to see how this continues to progress as a field,” says Kelly L. Stratton, MD FACS.